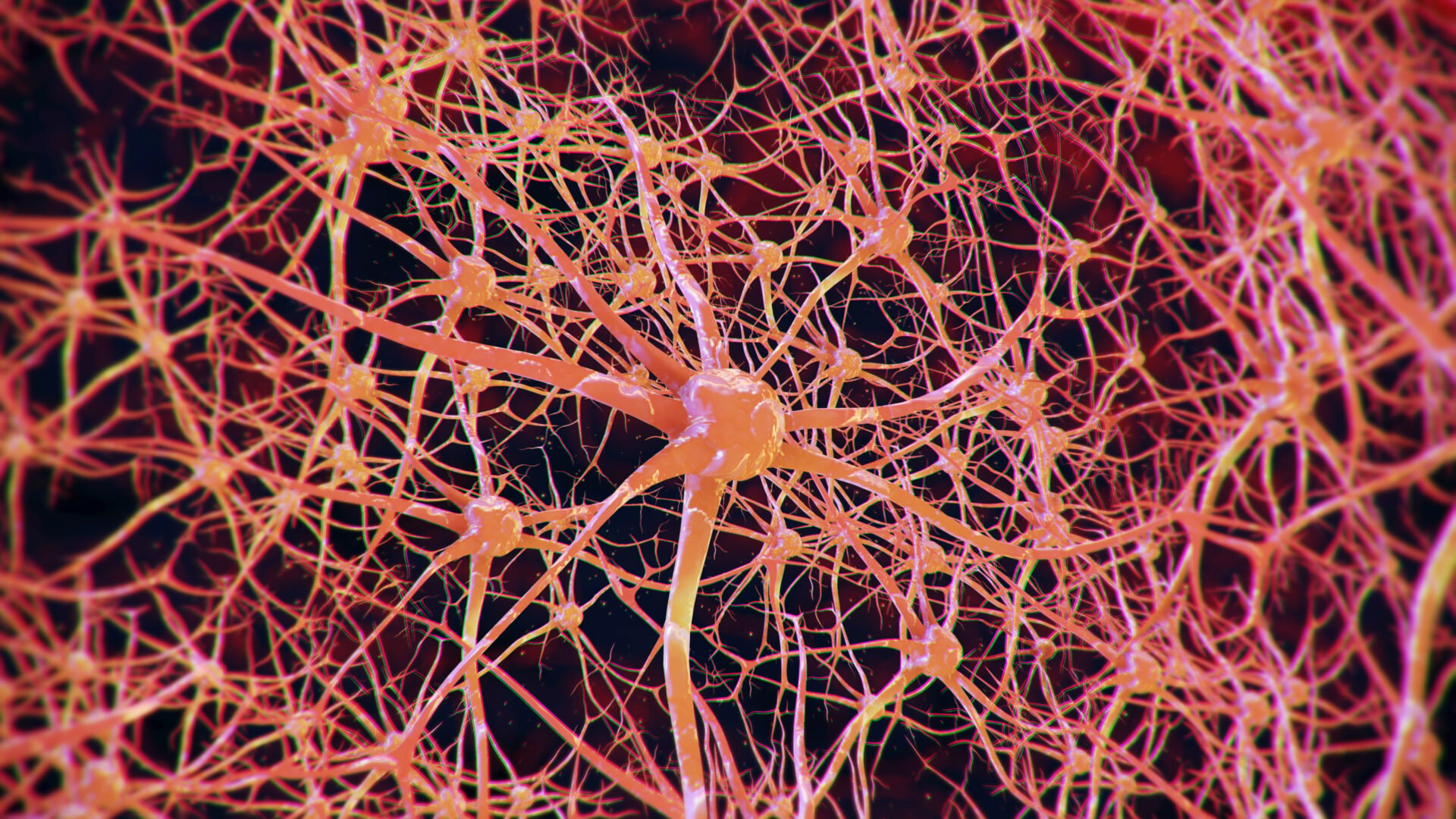
Despite the difficult times that have existed in recent years, both the treatment and the journey of people living with and affected by MS have continued to evolve. New data on the management of MS and related diseases was therefore presented at the joint ECTRIMS and ACTRIMS conference. The pathophysiology is gradually being better understood, leading to more targeted treatment for those affected.
Multiple sclerosis (MS) is a heterogeneous disease whose course is difficult to predict. Many models for predicting MS use peripherally collected blood, which is informative but may not capture the subtle disease changes in the CNS that are more indicative of disease progression. It was hypothesized that by measuring intrathecally synthesized proteins involved in inflammation, glial activation and CNS damage, predictive models for disease activity can be established. To determine how intrathecal proteins relate to short-term disease activity in relapsing-remitting MS (RRMS), intrathecal synthesis of 46 inflammatory mediators and 14 markers of CNS injury or glial activation was measured in matched serum and CSF samples from 47 MS patients undergoing diagnostic lumbar puncture [1].
All patients were followed for 12 months in a retrospective follow-up study and finally categorized as active (development of clinical and/or radiological disease activity within the first year of follow-up) or inactive (no disease activity). 27 patients with non-inflammatory neurological diseases (NIND) were included as negative controls. Data were subjected to differential expression analysis and network modeling to define neuroinflammation and CNS damage relevant to short-term disease activity in RRMS. The network analysis revealed a clear positive association between IgG1 and CXCL10, which is related to disease activity within 12 months. The analysis of disease activity-free survival showed that patients without IgG1-CXCL10 correlation have a better disease activity-free survival rate than patients without a significant correlation.
Differential diagnostics using MRI
The differential diagnosis of Susac syndrome (SuS), multiple sclerosis (MS) and primary angiitis of the central nervous system (PACNS) is still difficult in clinical practice. Magnetic resonance imaging (MRI) is a valuable tool for the diagnosis of these diseases, but the interpretation can be complex. Therefore, SuS patients from a Latin American cohort were compared with data from MS and PACNS patients [2]. The sample was divided into a training group and a test group. The training group was trained with the variables that independently showed predictive power for the outcome “SuS diagnosis” and a multivariate logistic regression model was performed. The coefficients obtained for each variable in the multivariate logistic regression model were rounded to whole numbers to assign a score value to the presence of each characteristic in the MRI.
The study included 46 SuS, 37 MS and 19 PACNS patients. Logistic regression analysis showed that “snowballs”, “spokes”, involvement of the corpus callosum and internal capsular lesions resembling a string of beads increased the probability of SuS as the final diagnosis, while the presence of Dawson fingers negatively predicted the diagnosis. The diagnostic score included three points for snowballs, two points for spokes, one point each for impairment of the corpus callosum and internal capsule, and five points were deducted if Dawson’s fingers were present. The cut-off for the SuS diagnosis was set at ≥5 points. High sensitivity (83%), specificity (100%) and accuracy (94.7%) were found in discriminating between SuS in MS and PACNS conditions.
Focus on NMOSD treatment
Neuromyelitis Optica Spectrum Disease (NMOSD) is a chronic autoimmune disease characterized by recurrent seizures in the central nervous system, resulting in permanent neurological damage and cumulative disability that affects health-related quality of life. A robust and rigorous trial comparison between two current NMOSD therapies, inebilizumab and satralizumab, was performed with a Matching Adjusted Indirect Comparison (MAIC ) using committee-assessed seizures to support an informed, evidence-based treatment decision [3]. An anchored MAIC compared the relative efficacy of inebilizumab with eculizumab and satralizumab based on published data from randomized control trials in adults with aquaporin-4-seropositive (AQP4+) NMOSD.
The relative risk of an NMOSD attack with inebilizumab compared to eculizumab and satralizumab was 1.51 and 0.49 respectively. The calculated life years showed an advantage for inebilizumab (21.90) compared to eculizumab (16.02) and satralizumab (20.79). There was also an advantage for inebilizumab (12.55) compared to eculizumab (8.23) and satralizumab (11.34) in terms of quality-adjusted life years. Using IAA to analyze the relative risk of NMOSD attack showed stronger results for treatment with inebilizumab than previously reported. In addition, treatment with inebilizumab produced better results for expected life years and quality-adjusted life years compared to satralizumab or eculizumab. The relative efficacy and discontinuation of treatment were the most important factors for the results.
Gender-specific differences in MS
There is a strong sexual dimorphism in multiple sclerosis (MS), which is reflected in the experimental TCR1640 mouse model of MS: Females have a relapsing-remitting disease, while males have a progressive disease phenotype. It has recently been shown that the sex of the adoptively transferred immune cells and not the sex of the recipient mouse is the primary determinant of the disease phenotype in this model. To gain a better understanding of the molecular determinants of this sex-specific observation, the transcriptomic signatures of the infiltrating immune cells of the central nervous system (CNS) need to be characterized. The aim of one study was therefore to investigate the gene signatures responsible for the sex-specific differences in infiltrating CNS immune cells in the experimental autoimmune encephalomyelitis (EAE) model of MS [4]. For this purpose, an adoptive transfer of immune cells from five male and six female TCR1640 mice into wild-type SJL/J mice was performed. At disease onset, seven days after transfer, CNS-infiltrating immune cells were isolated from male and female mice and processed for single-cell RNAseq (scRNAseq) with 10x Genomics and analyzed with Seurat.
After preprocessing, 87,121 CNS-infiltrating immune cells were found and 18 different cell clusters were identified based on transcriptomics. The hierarchical clustering of the samples based on the proportion of these 18 clusters showed a good separation of men and women. Given the putative role of T cells in EAE, T cells were extracted, regrouped and six T cell subpopulations were identified using ScType. Principal component analysis (PCA) based on the proportion of these newly clustered T cells again revealed a clear separation of immune cells between men and women. Interestingly, a significantly higher number of CD8+ T cells infiltrating the CNS was observed in males than in females. In contrast, women had a significantly higher number of CD4+ and regulatory-induced T cells compared to men. These results indicate a strong sex-specific determinant in the transcriptome and the relative abundance of CNS-infiltrating immune cells.
CSF antibodies in PPMS
Recently, CSF antibodies from patients with primary progressive multiple sclerosis (PPMS), when injected into mice, were found to be associated with the clinical and pathological features of the disease. This was not observed with CSF antibodies from patients with relapsing or secondary progressive MS. However, the specificity of these PPMS-associated antibodies or their mechanisms of action have not yet been clarified. CSF from MS patients was obtained by lumbar puncture and individual cells were isolated by FACS.
The heavy and light chains of the individual cells were sequenced by PCR and expressed and purified in plasmid vectors to generate recombinant antibodies. The antibodies, which are associated with motor weakness, demyelination and astrogliosis in experimental models, were tested for reactivity to a human proteomic microarray screening platform. All identified target molecules were then further analyzed for reactivity by Western blot and immunohistochemistry [5].
Reactivity against TIA1, an RNA-binding protein associated with cytotoxic granules, AKR7A3, a protein of the aldo-keto reductase family, and LAPTM4A, a lysosomal protein of transmembrane 4, was detected. Further tests with these pathogenic antibodies in the experimental rodent model could lead to a better understanding of their mechanism of action.
Inflammation in pMS
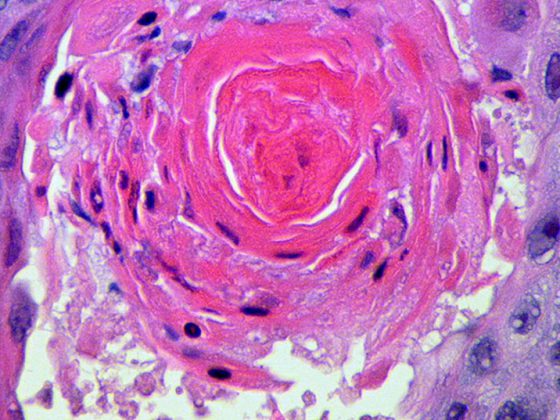
Chronic compartmentalized inflammation in niches of the central nervous system such as the leptomeninges, perivascular spaces and the choroid plexus plays a key role in the pathogenesis of progressive multiple sclerosis (pMS). Specifically, high levels of meningeal inflammation were found to be associated with a substantial “surface-in” gradient of neuronal loss and microglial activation in GML and NAGM with early and severe disease progression. The aim was to better characterize the inflammation by establishing immune-related gene profiles of meningeal infiltrates in pMS [6].
Formalin-fixed, paraffin-embedded (FFPE) sections from 60 postmortem progressive MS cases and ten healthy donors were used for immunohistochemical and morphometric analyses of the number, phenotype and localization of immune cells in the meninges. Six MS cases with marked meningeal inflammation and three control subjects were selected to use a new technology (CARTANA on a Nikon Ti2-E microscope with single-cell resolution) that enables in situ gene sequencing analysis (ISS) of a selected pool of 157 immune-related genes. In this technique, the mRNA is sequenced directly in the selected region of interest (ROI: meningeal infiltrate).
A detailed analysis of the meningeal cell count showed a significantly increased number of B cells in 26 of the 60 MS cases examined (43%), which were characterized by the highest degree of meningeal inflammation. In particular, the number of B cells was higher than that of macrophages and T cells. The ISS analysis revealed a significant increase in 85 of the 157 genes examined in MS-inflamed meninges compared to controls. Analysis of the KEGG pathways revealed that these genes are mainly associated with the interaction of viral proteins with cytokine/cytokine receptors, B cell receptor signaling, PD-L1 expression and PD-1 checkpoint pathways, and TNF signaling. Gene Ontology analysis revealed that most of the biological processes associated with these molecules involve regulation of the type 2 immune response, regulation of dendritic cell chemotaxis, membrane fusion involved in virus entry into the host cell, and regulation of T cell activation and polarization.
This suggests that highly specialized immune and inflammatory responses, possibly involving antiviral immunity, persist in the meninges of progressive MS and maintain intrathecal chronic inflammation.
Congress: 9. Kongress der European und American Committee for Treatment and Research in MS (ECTRIMS-ACTRIMS) 2023
Literature:
- Welsh N, et al.: Correlation of intrathecal levels of IgG1 and CXCL10 predict disease activity in multiple sclerosis. P004/2117. MSMilan2023 – Paper Poster – Session 1. Multiple Sclerosis Journal 2023.
- Marrodan M, et al.: Diagnostic MRI score to differentiate Susac Syndrome from Multiple Sclerosis and Primary Angiitis of the Central Nervous System. P007/864. MSMilan2023 – Paper Poster – Session 1. Multiple Sclerosis Journal 2023.
- Paul F, et al.: Matching-Adjusted Indirect Comparison of Current Treatments for NMOSD and Evaluation of Long-Term Effectiveness. P011/1038. MSMilan2023 – Paper Poster – Session 1. Multiple Sclerosis Journal 2023.
- Rébillard RM, et al.: Transciptomic signatures of infiltrating immune cells underpinning sex differences in experimental autoimmune encephalomyelitis. P111/1380. MSMilan2023 – Paper Poster – Session 1. Multiple Sclerosis Journal 2023.
- Lin J, et al.: Investigation of cerebrospinal fluid antibody specificity in primary progressive MS. P120/2316. MSMilan2023 – Paper Poster – Session 1. Multiple Sclerosis Journal 2023.
- Mastantuono M, et al.: Combined neuropathology and in situ sequencing characterization of meningeal inflammation in progressive multiple sclerosis. P121/1630. MSMilan2023 – Paper Poster – Session 1. Multiple Sclerosis Journal 2023.
InFo NEUROLOGIE & PSYCHIATRIE 2023; 21(6): 34–35