If clinically suspected, hepatocellular carcinoma is diagnosed using laboratory parameters, imaging and, if necessary, a biopsy. In particular, contrast-enhanced imaging procedures such as sonography, computer tomography and magnetic resonance imaging play an important role in diagnosis and follow-up.
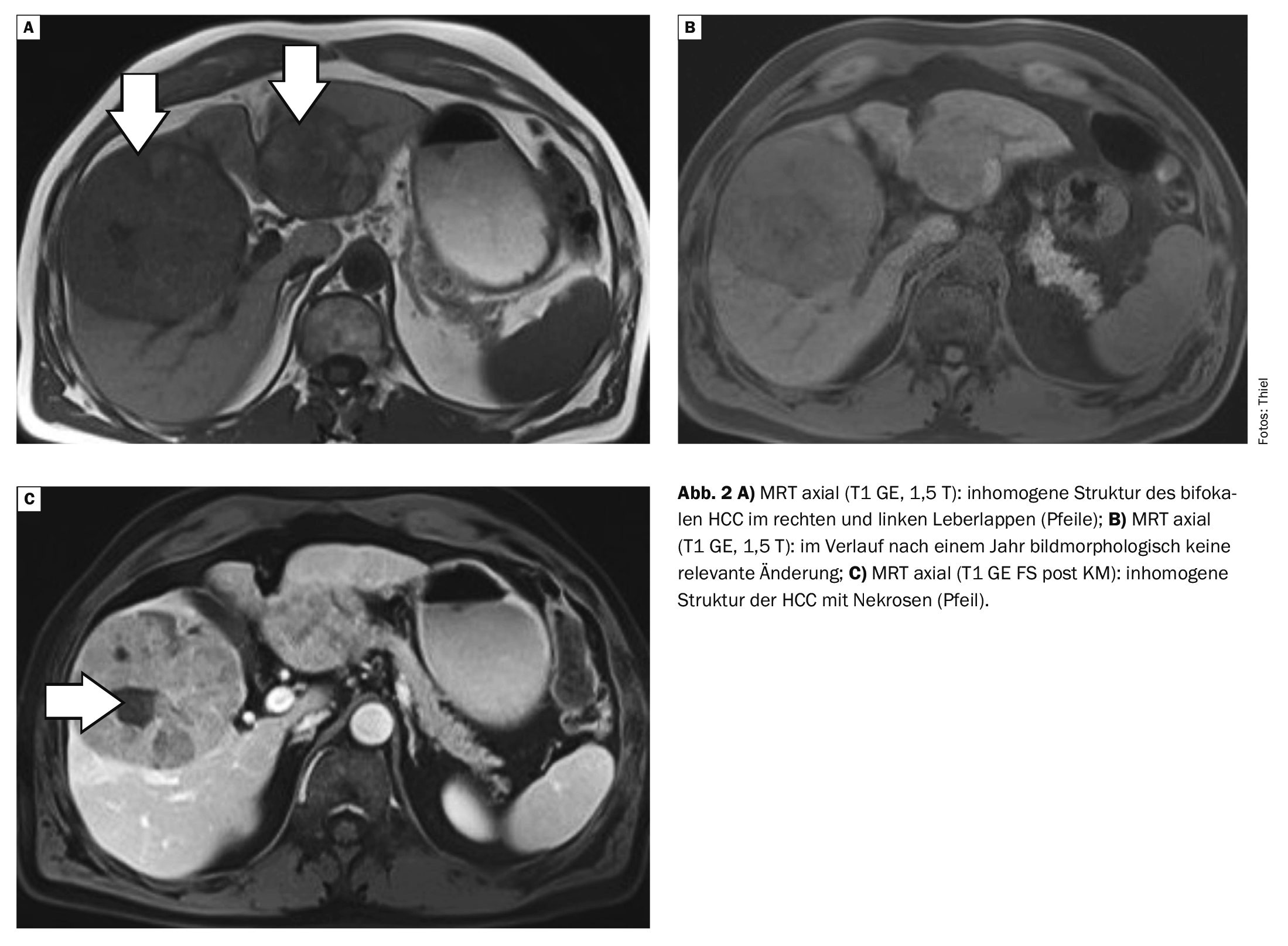
The incidence of hepatocellular carcinoma (HCC) in Western Europe is relatively low at around 5:100,000 per year. In large parts of Asia and Africa, the incidence is much higher at 5-30% due to the increased prevalence of chronic viral hepatitis and a tendency towards an earlier age of onset. Men fall ill about 3-4 times more frequently than women [1,2]. Various pre-existing conditions and risk factors favor the development of HCC, as shown in Table 1.
In hepatocellular carcinoma, a distinction is made between three growth forms, which are listed in Table 2.
All forms of hepatocellular carcinoma tend to invade surrounding blood vessels. Tumor cones can thus break into the vena portae or inferior vena cava and obstruct the lumen of the vessels. Metastases occur relatively late in the course of the disease and then primarily affect the regional lymph nodes, lungs, bones and adrenal glands.
Clinically, there are initially unspecific general symptoms such as nausea, vomiting and loss of appetite. Pressure pain in the right upper abdomen is usually an expression of capsular tension in the liver. In advanced stages, a palpable tumor can be detected in the right upper abdomen, as well as ascites and cachexia.
Occasionally, hepatocellular carcinoma manifests itself through decompensation of an existing liver cirrhosis and/or through paraneoplastic symptoms such as fever.
Laboratory, imaging and possibly also tissue clarification are important diagnostically, and liver transplantation is the therapeutic option of choice with a curative approach. Palliative transarterial chemoembolization and concomitant antiviral therapy for hepatitis B and C can be used as secondary prevention [3].
Contrast-enhanced imaging techniques (sonography, computed tomography and magnetic resonance imaging) show a relatively precise delineation and classification of the tumor. HCC is characterized by an accumulation of contrast medium (hyperperfusion) in the arterial phase with subsequent rapid wash-out in the portal venous and venous phase. A further criterion is a size of the mass of >1 cm. MRI has a higher sensitivity than CT, especially for smaller lesions, so MRI should be performed first and foremost. In the case of unclear, small (<1 cm) masses, a follow-up examination after three months is recommended. However, if the mass is larger than 1 cm and shows atypical contrast agent behavior, either detection in a second imaging scan or a biopsy is mandatory to establish a reliable diagnosis before starting treatment. As the symptoms only appear relatively late, HCC is often detected late. The death rate currently shows an annual increase of 2-3% worldwide [4].
X-rays have no significance for the detection of hepatocellular carcinoma.
Magnetic res onance imaging has a high sensitivity in the detection of HCC. The use of contrast agents in magnetic resonance imaging for the diagnosis of hepatocellular carcinoma is mandatory. The aim of current research is the use of MR sequences without the use of contrast agents [5].
Computed tomography scans have assumed a supplementary position in the diagnostic procedure. If the MRI findings are unclear, triphasic CT and/or contrast-enhanced ultrasound should be used [6].
In order to detect suspicious HCC changes at an early stage, patients at risk should undergo sonography every six months [7]. Depending on its size, HCC is often visualized with a mixed echo pattern, with smaller HCC lesions under 3 cm usually being visualized hypoechogenically. Hypervascularization can be demonstrated by Doppler and power Doppler sonography. Arterial hypervascularization and the subsequent rapid wash-out can be visualized with contrast-enhanced sonography.
Case studies
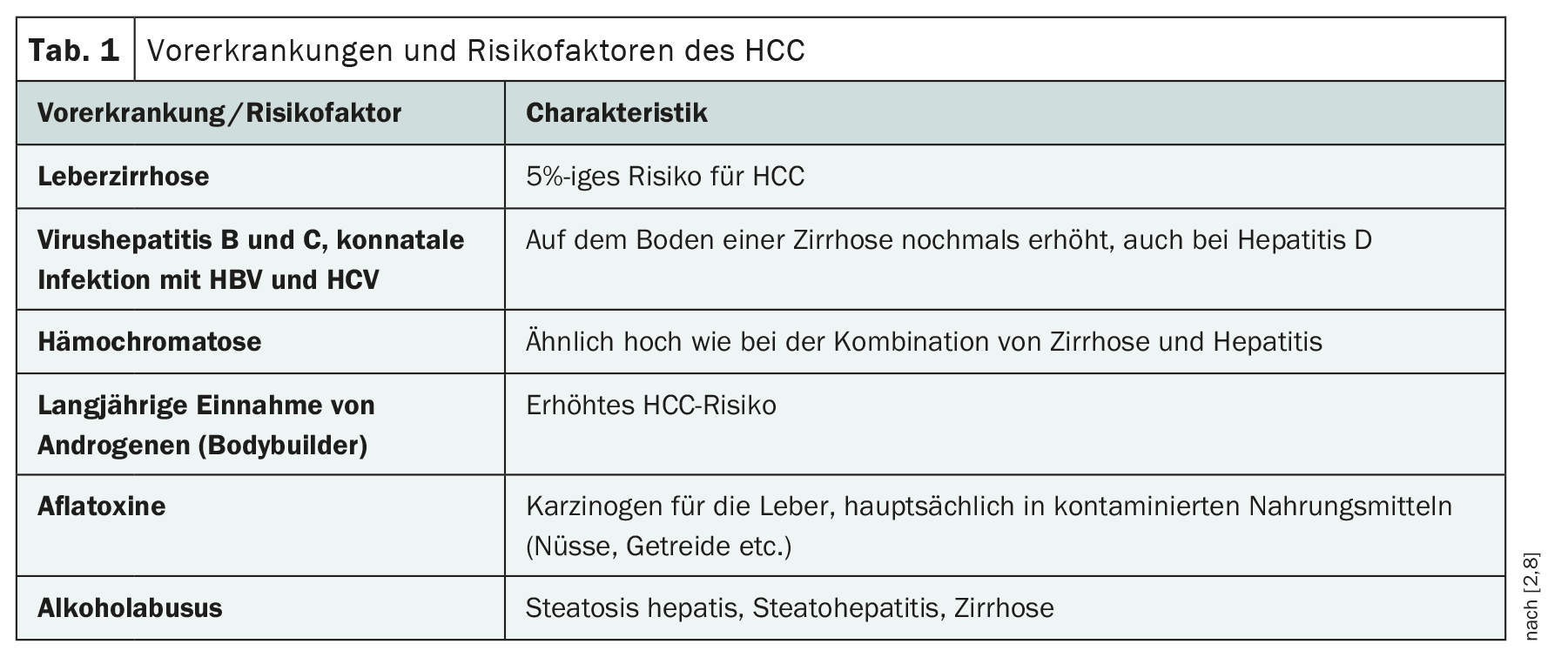
Case study 1 shows the progression of hepatocellular carcinoma in a 68-year-old patient. The initial diagnosis was made in April 2022. The therapeutic measures included TIPPS and chemoembolization. Post-therapeutic CT monitoring in February 2024 demonstrated not only HCC but also significant splenomegaly and surrounding portocaval circulation (Fig. 1A to C).
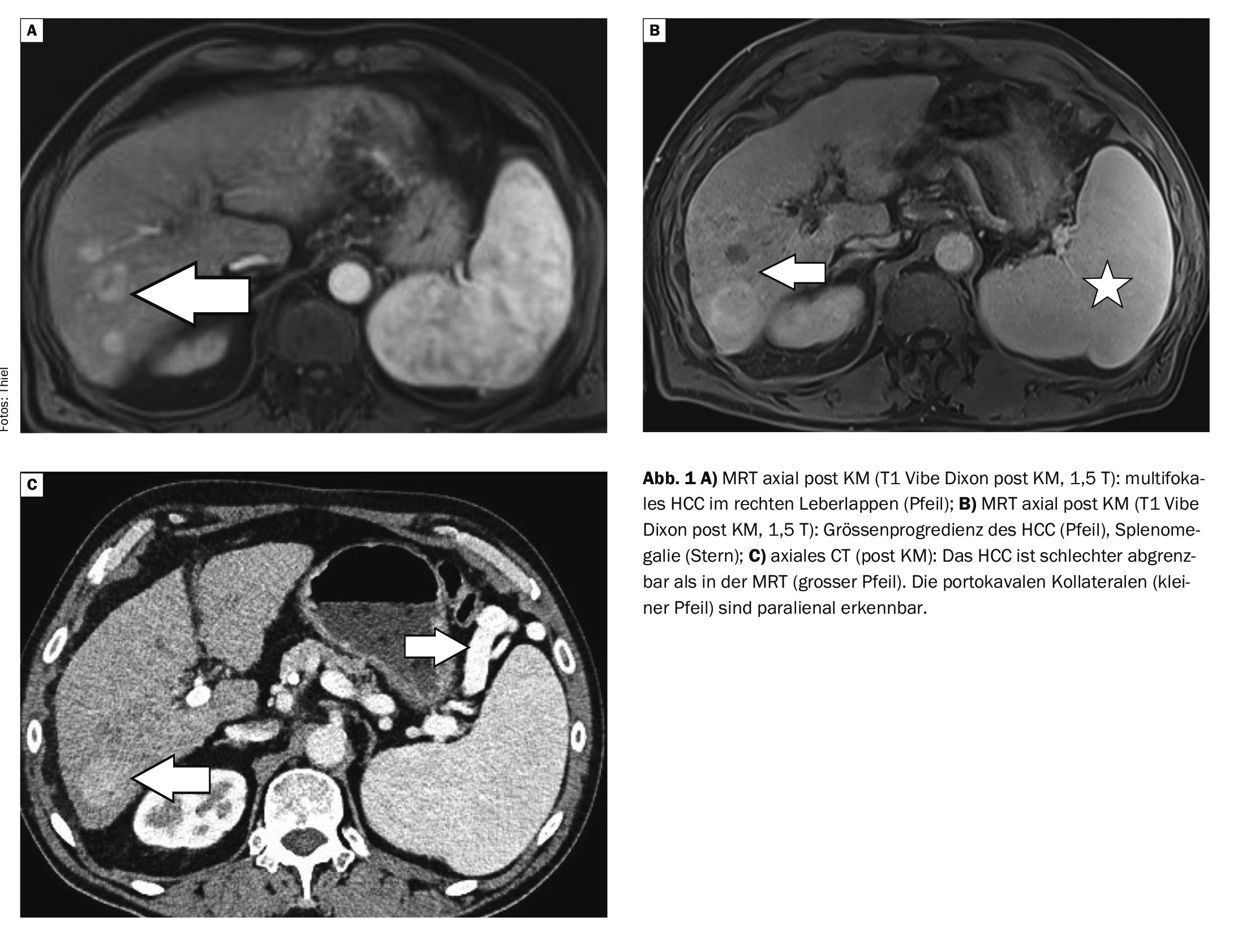
Case study 2 shows the follow-up of an HCC under sorafenib therapy. The MRI in April 2015 showed a bifocal tumor in the right and left lobe of the liver. The follow-up MRI 1 year later demonstrates increasing necrosis of the masses with almost unchanged tumor size (Fig. 2A to C).
Take-Home-Messages
- The incidence of hepatocellular carcinoma in Western Europe
is low. - Men are affected more frequently than women.
- Several pre-existing conditions and toxins such as viral hepatitis B and C and alcohol abuse significantly increase the risk of developing HCC.
- There are different forms of growth.
- A combination of laboratory, imaging and occasionally biopsy is usually required to make a diagnosis.
Literature:
- Burgener FA, et al: Differential diagnostics in MRI. Georg Thieme Verlag Stuttgart, New York: 2002; pp. 500-502.
- Hircin E, et al: Hepatocellular carcinoma. https://flexikon.doccheck.com/Hepatozelluläres_Karzinom,(last accessed 03.07.2024)
- Urbanek P, Hribek P: Hepatocellular carcinoma from the view of gastroenterologist/hepatologist. Clinical Oncol 2020 Fall; 33(Supplement 3): 34-44.
- Wang W, Wie C: Advances in the early diagnosis of hepatocellular carcinoma. Genes Dis. 2020; 7(3): 308-319.
- Niendorf E, et al: Contrast Enhanced MRI in the Diagnosis of HCC. Diagnostics (Basel) 2015, Sep 21; 5(3): 383-398.
- S3 guideline Diagnostics and therapy of hepatocellular carcinoma and biliary carcinoma, 2021. https://leitlinienprogramm-onkologie.de,(last accessed 03.07.2024)
- Lincke T, Boll D, Zech C. Radiology up2date 4; 2016: 295.
- Fu Y, et al: Alcohol-associated liver cancer. Hepatology 2024, Apr 12. doi: 10.1097.
- Smith M, Tomboc PJ, Markovich B: Fibrolamellar Hepatocellular Carcinoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan, 2022 Sep 26.
InFo ONCOLOGY & HEMATOLOGY 2024; 12(5): 26-28