Case report: An eight-day-old boy presents with new onset of blisters since three days. The child is in good general condition and afebrile. There were no abnormal findings in the internal status at admission. There is no known family history of skin disease.
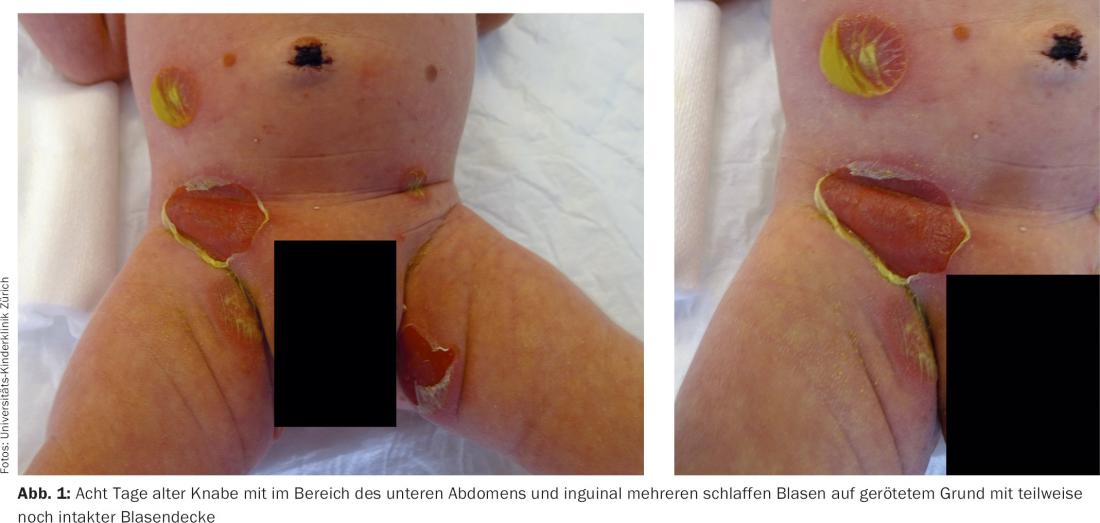
Clinical Presentation: Inguinal, gluteal, on the lower abdomen and on the right wrist, there are approximately 1-2 cm large, flaccid blisters as well as superficial erosions (Fig. 1) . The preserved blisters are serous filled, the mucous membranes are inconspicuous.
Quiz
Based on these findings, which is the most likely diagnosis?
A Bullous impetigo
B Staphylococcal Scalded Skin Syndrome
C Epidermolysis bullosa hereditaria
D Neonatal pemphigus vulgaris
E Epidermolytic ichthyosis
Diagnosis and Discussion: Based on the present findings, we made a diagnosis of bullous impetigo. Swabs were taken for microbiological diagnosis (nose, umbilicus, inguinal) and intravenous antibiotic therapy with clindamycin was initiated. Local treatment was with octenidine (Octenisept® Gel) alternating with mupirocin (Bactroban® Ointment). With the detection of Staphylococcus aureus in nasal, umbilical, and inguinal swabs, the diagnosis of bullous impetigo was confirmed.
Phage group II staphylococci (types 71 and 55) are causative agents of bullous impetigo and staphylococcal scalded skin syndrome (SSSS). The exfoliative toxins of S. aureus (ET-A and ET-B) play a central role in the development of blisters. They lead to a degradation of desmoglein 1 in the epidermis and thus to a gap formation at the level of the stratum granulosum. Due to the selectivity for desmoglein 1, analogous to pemphigus foliaceus, there is no involvement of the oral mucosa.
Usually, the diagnosis of bullous impetigo can be made clinically. Smear tests for microbiological pathogen diagnosis are useful. The clinical picture is characterized by fragile, yellow-serous to pus-filled blisters that rapidly rupture, leaving a rolled-up yellowish blister margin and superficial erosions that then crust over. Predilection sites for bullous impetigo in the newborn are the diaper region, axillae, and neck (Fig. 1). In disseminated forms, systemic antibiotic therapy is indicated; single foci can also be treated topically.
While bullous impetigo is a local skin infection without general clinical signs, SSSS involves hematogenous dissemination of exfoliative toxins from mostly extracutaneous foci of infection, often localized in the nasopharyngeal region or occult [1]. Typically, affected children have perioral, radially furrowed crusts and extensive, pouchy, painful erythema with secondary extensive exfoliation when severe ( Fig. 2).

Extensive blisters in the neonatal and infant period always represent an alarm symptom and require rapid referral to an institution experienced in the intensive care of young children. Besides bullous impetigo/SSSS, other infections (herpes simplex, varicella, etc.), autoimmune bullous dermatoses, genodermatoses (epidermolysis bullosa, epidermolytic ichthyosis), mastocytoses, severe drug reactions and others should be considered. In addition to microbiological examinations, laboratory tests (e.g., detection of autoantibodies) and a skin biopsy may be useful.
Literature:
- Handler MZ, Schwartz RA: Staphylococcal scalded skin syndrome: diagnosis and management in children and adults. J Eur Acad Dermatol Venereol 2014; 28(11): 1418-1423.
Further reading:
- George A, et al: Extensive pustules in a neonate. Diagnosis: impetigo neonatorum. Pediatr Dermatol 2014; 31(5): 609-610.
- Antaya RJ, Robinson DM: Blisters and pustules in the newborn. Pediatr Ann 2010; 39(10): 635-645.
- Hussain S, Venepally M, Treat JR: Vesicles and pustules in the neonate. Semin Perinatol 2013; 37(1): 8-15.
DERMATOLOGIE PRAXIS 2015; 25(5): 25-26










