Migraine is one of the most common of the more than 240 forms of headache and significantly restricts sufferers in their daily lives and quality of life. Although the number of patients is extremely high, the disease is often still underestimated and is undertreated. There are now effective ways of averting migraines before they start.
More than 136 million people worldwide are affected by migraine [1]. Both peripheral and central sensitization processes are involved in the underlying complex pathophysiology. A key role is played by calcitonin gene-related peptide (CGRP), the level of which rises in saliva during an attack and can also be detected elevated in the blood in chronic migraine. In a chronic form of the disease, the sufferer suffers from at least 15 headache days per month for more than three months, eight or more of which manifest as migraines. Until recently, oral medications such as antidepressants, antiepileptics, or beta-blockers were the main drugs available to control the disease at an early stage. However, more than 80% of chronic migraine sufferers discontinue oral prophylaxis within a year due to lack of efficacy or intolerable side effects [2,3].
Insights into pathophysiology
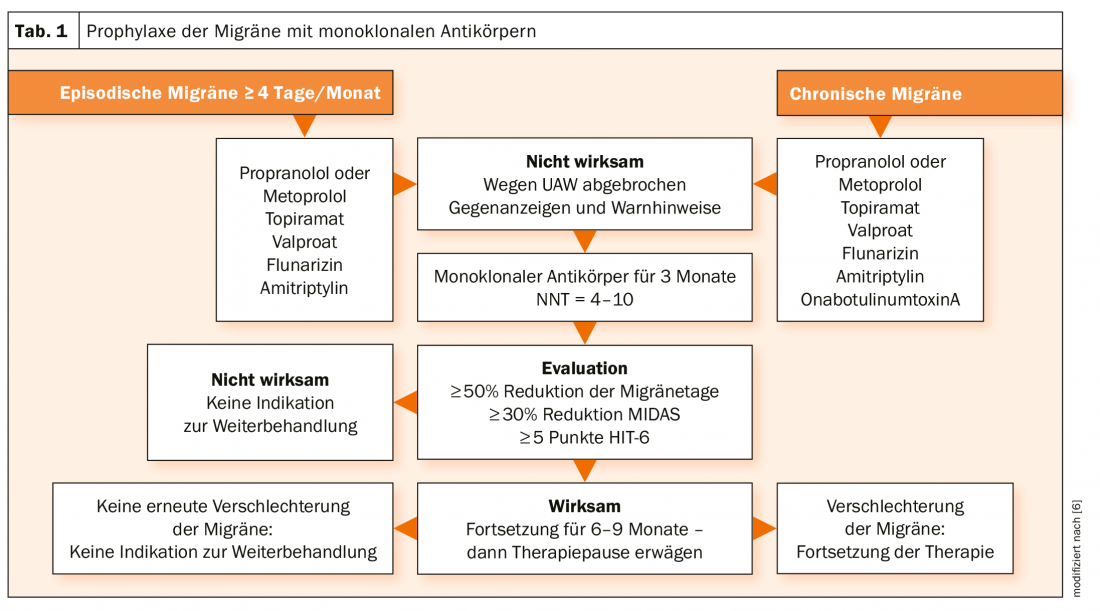
The aim of effective migraine prophylaxis is to reduce the number, severity and duration of migraine attacks (Table 1) . Indications include particular distress, reduced quality of life, and the risk of medication overuse. CGRP antibodies (fremanezumab, galcanezumab, eptinezumab) that specifically dock to the ligand of CGRP have been developed specifically for prevention. This prevents binding of CGRP isoforms to the receptor. Erenumab, on the other hand, binds to the CGRP receptor so that the neurotransmitter can no longer dock. This is because CGRP has been shown to play an important role in the pathophysiology of migraine. CGRP levels increase markedly during an attack and remain elevated in between, especially in the chronic form [4,5].
All study data to date demonstrate a very good benefit-risk profile for the currently available preparations. Side effects may include mainly pain or reaction at the injection site and nasopharyngitis. However, the effect is so convincing that dropout rates are very low. Good results can be achieved even in pretreated patients. The reduction in migraine days per month ranges from 4.3 to 6.6 days for chronic migraine. The responder rate after 3 months ranges from 27% to 57%. Efficacy has also been shown for patients with headaches caused by overuse of painkillers or migraine medications. In addition, effective efficacy with good tolerability has now also been demonstrated for a number of subgroups (e.g., depression, cardiovascular events).
Literature:
- Stovner LJ, Nichols E, Steiner TJ, et al: Lancet Neurol 2018; 17: 954-976.
- Hepp Z, Dodick DW, Varon SF, et al: Cephalalgia 2017; 37: 470-485.
- Blumenfeld AM, Bloudek LM, Becker WJ, et al: Headache 2013; 53: 644-655.
- Edvinsson L, Haanes KA, Warfvinge K, Krause DN: Nat Rev Neurol 2018; 14: 336-350.
- Cernuda-Morollon E, Larossa D, Ramon C, et al: Neurology 2013; 81:1191-1196.
- www.dgn.org/leitlinien/3859-ll-030-057-cgrp-addendum-migraene-leitlinie-2019 (last accessed on 25.05.2020)
InFo NEUROLOGY & PSYCHIATRY 2020; 18(4): 38 (published 6/30/20, ahead of print).











