For the light therapy of the atopical eczema relatively secured data can be fallen back. Moreover, numerous studies prove the favorable effect mechanisms of a stationary high mountain climatic skin treatment. For the future, an update of the data collection, e.g. concerning freedom from recurrence, use of medication and personal well-being after treatment in the high mountains – to name just a few parameters – is to be desired. Similarly, comparisons should be made to control groups treated in the lowlands.
Already in pre-Christian times, Hippocrates and others described the dependence of health on climatic factors [1]. A systematic study of the effect of phototherapy on atopic eczema was first performed in 1948 [2]. The currently still valid S2 guideline for the treatment of atopic dermatitis provides for the use of UV light – under consideration of the age limit – from stage 2 [3].
The rationale for this treatment modality can be briefly outlined as follows: Immunosuppression (affecting antigen-presenting Langerhans cells, infiltrating T cells, proinflammatory cytokines such as IL12, IL2, interferon alpha, TNF alpha, among others), increase in expression of antimicrobial peptides (beta-defensins, cathelicidins), and germ reduction (S. aureus, Pityrosporum ovale) [4].
In terms of side effects, the following situations must be considered: Dermatitis solaris, reactivation of herpes simplex viral disease, development of polymorphous light dermatosis, initiation of photocarcinogenesis (e.g., actinic keratosis, squamous cell carcinoma), folliculitis, facial hypertrichosis, photoonycholysis, and cataract.
Caution should also be exercised when considering UV therapy if the patient has a generally increased sensitivity to light, has a history of skin malignancy, is taking a photosensitizing drug, or has a seizure disorder [5].
In a systematic review of published UV studies up to 2011, Garritsen et al. [6] clearly identify mid-dose UVA1 and narrow-spectrum UVB exposure as first-line agents for atopic dermatitis therapy.
High mountain climate – meteorological factors
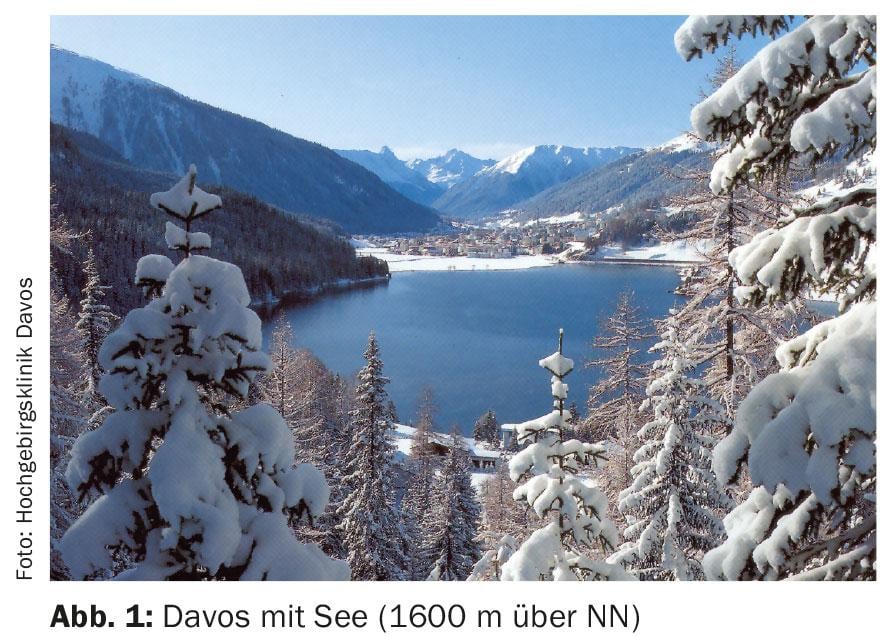
Efficient dermatologic-allergologic climatic therapy in the current sense appears to be useful only in climates with pronounced irritant factors [7]. Examples of such characterized locations are the North Sea islands or Davos (Switzerland) located at 1600 m above sea level (Fig. 1) . In climate therapy, effects due to the climate itself must be separated from effects due to therapy in the climate [8].
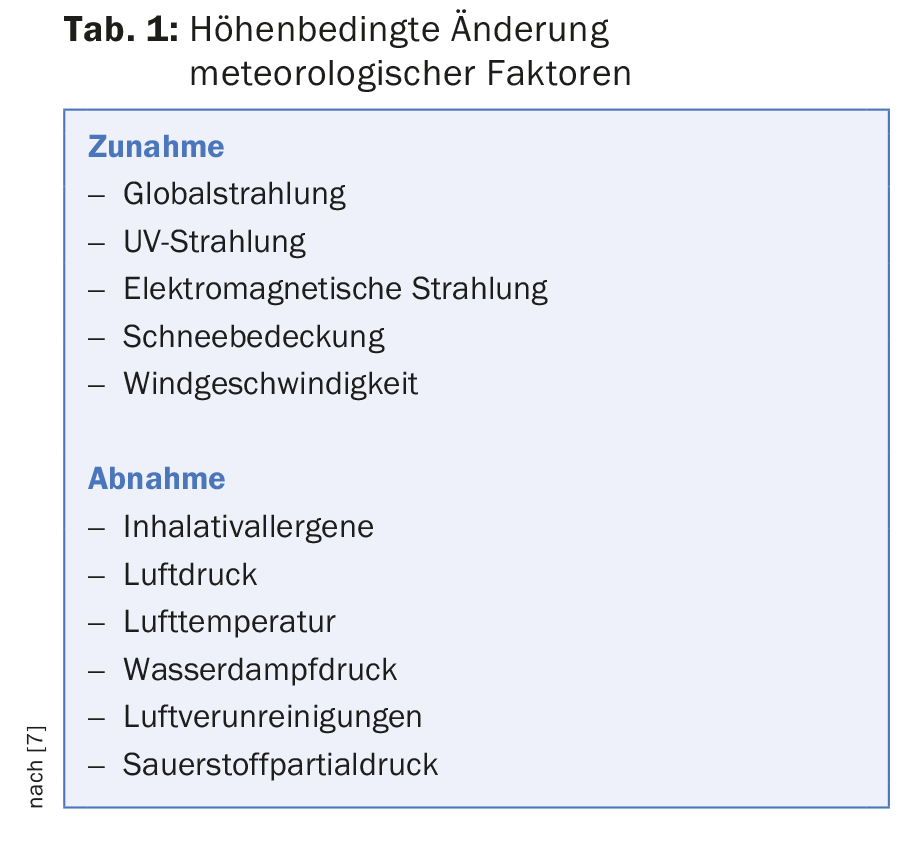
Depending on the altitude, significant environmental parameters change. Table 1 provides an overview.
The special radiation climate in the high mountains – with increase of daily sunshine duration above 800 m in autumn and winter, higher global radiation and intensity increase of the wavelength range of 290 and 350 nm, which is significant for dermatotherapy – can be used in the form of heliotherapy almost all year round. Even with cloudy skies, residual radiation that can be used therapeutically still reaches the exposed skin-suffering patient [7].
A lowered oxygen partial pressure, as it exists in the high mountain climate compared to the lowlands, causes a circulatory activation, a deepening of the respiration as well as an improvement of the skin blood circulation, which is used therapeutically.
Decreased humidity at altitude leads to increased evaporation through the skin, a decrease in skin temperature and a reduction in itching.
Furthermore, the lack of sultriness in the high mountain climate leads to reduced sweat and heat stress on the skin organ.
The protected high-mountain valley location of Davos is also held responsible for the fact that a reduced number of infectious pathogens – compared to lower-lying regions – can be detected there [7].
The often considerable distance from the place of residence or work also has positive effects on the psyche and skin.
Allergen situation
Above 1500 meters of altitude it can be assumed that the house is free of dust mites. Other potent allergens (e.g. birch and grass pollen, mold spores) are significantly reduced in concentration as well as in the duration of their occurrence or are almost completely absent. Figure 2 shows for the concentration of birch pollen (average annual pollen sum) the differences for Basel (273 m above sea level), Samedan (1705 m above sea level) as well as Davos (1600 m above sea level).
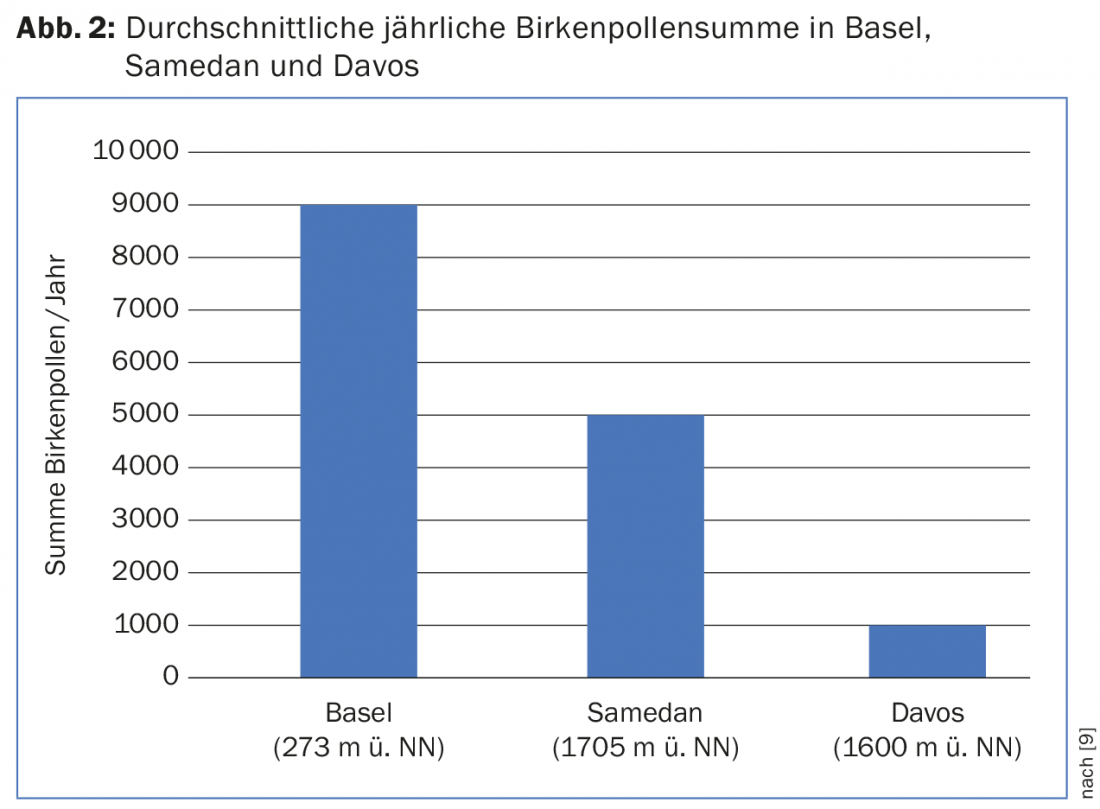
Interestingly, Samedan, which is located at a higher altitude than Davos, has higher pollen concentrations [9]. This is associated with relatively seen less favorable site conditions of Samedan (such as increased aerogenic pollen supply due to meteorological and geographic features).
Data situation
In a catamnestic follow-up study from 1961 to 1995, the discharge status of 31 438 neurodermatitis patients after inpatient treatment in Davos was recorded by dermatologists [7]. In 96.7%, the findings were free of symptoms or significantly improved, in 2.8% they were unchanged, and in 0.5% they worsened.
A catamnestic follow-up from January 1995 to July 1996 showed the following result after evaluation of 624 patient questionnaires: During the high mountain climate therapy in Davos, a topical glucocorticoid in use before the start of treatment could be discontinued in two thirds of the patients. One year after climatic therapy in Davos, 70% of patients reported using no or less cortisone-containing topicals than before admission [10].
An investigation of the Zurich working group around Wüthrich [11] could state after an on the average 32-day stationary climatic therapy in Davos a symptom freedom and/or clear finding improvement with 89% of the 97 examined adult patients with Neurodermitis. 74% of patients who were unable to work before treatment began were able to resume work after the inpatient intervention. There were also significant differences in medication use: before the start of therapy, 73% used steroids, of which 14% used systemic therapies. At the end of therapy, topical steroids could be discontinued in 71% and all systemic corticosteroids in almost all cases [11].
A similar picture was seen in children: of 375 children with atopic eczema, topical corticosteroids could be discontinued in 225 children (60%) during high mountain climate therapy in Davos. Within the first year after treatment in Davos, two-thirds of the children did not require external cortisone. Of those who had to be retreated with topical cortisone during this period, about 60% came off with weaker-acting steroids and with lower amounts of steroids [12].
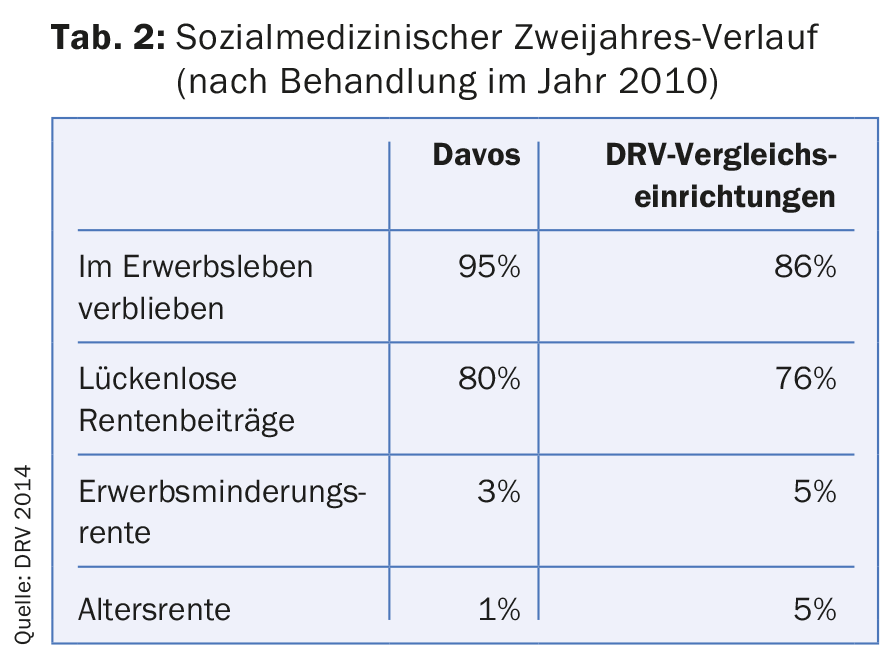
In a survey from the period January 1 to 31. December 2010, 128 adults with skin diseases (predominantly patients with neurodermatitis, but also psoriasis vulgaris, etc.) who had been treated in the Davos High Mountain Clinic were compared with 23 480 adults with the disease who had been treated in other clinical facilities of the German Pension Insurance (DRV). In the two years following completion of the rehabilitation measure, the inpatient measure in Davos was found to be superior to the other DRV facilities in terms of important socio-medical parameters (tab. 2).
Contraindications
General medical contraindications to climatic therapy are decompensated cardiovascular diseases, severe liver and kidney diseases, florid infectious diseases, severe endocrinological disorders and manifest psychiatric diseases.
On the part of dermatology, contraindications include: concurrent light dermatoses and general high-grade hypersensitivity to light [4].
Literature:
- Vocks E: Climatotherapy in atopic eczema. In: Ring J, Przybilla B, Ruzicka T (eds.): Handbook of Atopic Eczema. 2nd ed. Heidelberg, Springer 2006; 507-523.
- Nexmand PH: Clinical studies of Besnier’s prurigo (diss.). Copenhague, Rosenkilde and Bagger 1948.
- Werfel T, et al: Neurodermatitis S2 guideline. JDDG 2009; 7(Suppl. 1): S1-S49.
- Ring J, et al: Guidelines for treatment of atopic eczema (atopic dermatitis) Part II. JEADV 2012; 26: 1176-1193.
- Sidbury R, et al: Guidelines of care for the management of atopic dermatitis. Section 3. management and treatment with phototherapy and systemic agents. JAAD 2014; 71: 327-349.
- Garritsen FM, et al: Photo(chemo)therapy in the management of atopic dermatitis: an updated systematic review with implications for practice and research. BJD 2014; 170: 501-513.
- Engst R, Vocks E: High mountain climate therapy for dermatoses and allergies – mechanisms of action, results and immunological parameters. Rehabilitation 2000; 39: 215-222.
- Vocks E, Engst R, Karl S: Dermatological climatotherapy-definition, indications, and health policy necessity. Rehabilitation 1995; 34: 148-153.
- Gehrig R, Peeters AG: Pollen distribution at elevations above 1000 m in Switzerland. Aerobiologica 2000; 16: 69-74.
- Duve S, Walker A, Borelli S: Follow-up of neurodermatitis constitutionalis atopica during high altitude climate therapy. Dt Derm 1991; 39: 1418-1428.
- À Porta B, Barrandun J, Wüthrich B: Neurodermatitis atopica – therapy in a high mountain climate. Praxis (Bern) 2000; 89: 1147-1153.
- Heine A: Course and cortisone medication in childhood atopic diseases after high mountain climate therapy. Inaugural Dissertation, Technical University of Munich 1995.
DERMATOLOGIE PRAXIS 2015; 25(6): 19-22