The cardiovascular benefit of SGLT2 inhibitors and GLP1 analogues is now considered established, and non-diabetics may also benefit. For optimal results, therapy should be tailored to individual patient characteristics.
Intervention studies in previous years have shown that blood glucose control can reduce the incidence of microvascular complications, but other factors play a greater role in macrovascular complications, explains Fabian Meienberg, MD, Head of Endocrinology & Diabetology, Baselland Cantonal Hospital [1]. More than ten years ago, there was a controversy about whether rosiglitazones (oral antidiabetic drugs from the group of insulin sensitizers) lead to increased cardiovascular events. Subsequently, this substance was withdrawn from the market, and from that point on the FDA required that blood glucose-lowering drugs also be evaluated for safety with respect to cardiovascular events.
This led to the Cardiovascular Outcome Trials (CVOT), in which MACE (major adverse cardiac event) was examined as the primary endpoint in randomized-controlled clinical trials of the new antidiabetic drugs. EMPA-REG was the first of these cardiovascular endpoint studies to be designed in a non-inferiority design – the primary objective was to demonstrate that no greater number of cardiovascular events occurred than with standard-of-care. The EMPA-REG study data published in 2015 [2] were a minor revolution in the field of diabetology, he said. It has been shown that the SGLT2 inhibitor empagliflozin, in addition to glucose lowering, also leads to a significant reduction in the risk of MACE in diabetic patients and also reduced the risk of mortality over an observation period of three years [2]. Cardiovascular risk reduction was roughly comparable to statins or ACE inhibitors. “This is very impressive data,” Dr. Meienberg said.
Cardioprotective effects not mediated via glycemic control
SGLT2 inhibitors and GLP1 analogs are the two currently available drug classes with additional cardiovascular benefit. The cardiac benefit of the new antidiabetic agents has been considered in recent guidelines from various European and North American professional societies [3–6]. When prescribing antidiabetic therapy, therefore, additional criteria are now relevant in addition to blood glucose control.
“From the results of various cardiovascular outcome trials, it appears that SGLT2 inhibitors and GLP1 analogs have a significant effect on MACE, whereas DPP4 inhibitors do not,” the speaker explained. The exact mechanisms of action are not yet fully understood. For GLP1 analogues, it is debated whether promotion of weight loss is related; for SGLT2 inhibitors, hemodynamic changes are more likely to be the driving force. However, these hypotheses are rather speculative at this point in time and are not empirically supported. Follow-up studies of CVOTs have tested the efficacy of the new agents in subjects without diabetes (e.g., SGLT2 inhibitors in heart failure patients as add-on treatment). Positive effects on cardiovascular endpoints were found to be independent of whether they were type 2 diabetics, and renal function scores did not appear to play a role in this. This was evidence that the cardiovascular protective effect of SGLT2 inhibitors was not due to blood glucose lowering.
Several individual target values in focus
For optimal treatment results, a treatment regimen tailored to individual patient characteristics is promising (Overview 1). For example, if a patient has known heart failure, the speaker advises the use of SGLT2 inhibitors, regardless of BMI. If there is no heart failure and a BMI>28, he would lean more toward the GLP1 analog. In addition to the newer drug classes (SGLT2 inhibitors, GLP1 analogs, DPP4 inhibitors), metformin is still considered the standard of first-line therapy according to current consensus recommendations. Metformin is a well-established and proven substance that also has some additional cardiovascular benefit, although not as pronounced. “Sulfonylureas and glitazones should now only be used when cost-effectiveness of treatment is a key factor.” Which substance class is best suited for which patient depends on individual target values and criteria:
BMI: GLP1 analogues are currently most effective in high BMI. The appetite suppressant effect of GLP1 analogues such as liraglutide (e.g. Victoza®, [7]) is also approved as a preparation for weight control under the drug label Saxenda® [8]. Some patients would benefit enormously from this substance class, the speaker is of the opinion that GLP1 analogues are currently prescribed rather too rarely. “In high BMI, GLP1 analogs are the substance with potentially the greatest benefit.”
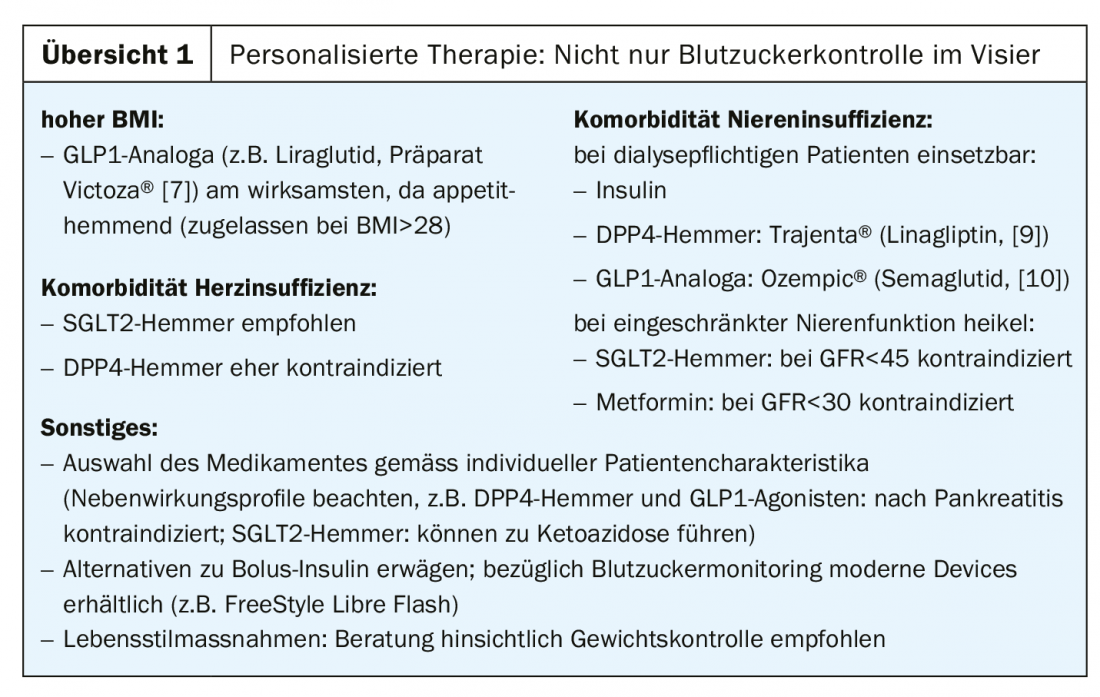
Heart failure: SGLT2 inhibitors are preferable. The patient derives a similar benefit from it as from an ACE inhibitor. DPP4 inhibitors have shown a mildly negative effect in this regard in patients with heart failure, which is why they tend not to be used in patients with known heart failure.
Renal failure: According to new data, SGLT2 inhibitors are suitable because they are nephroprotective – as in heart failure, this effect seems to be independent of diabetes status. Among the DPP4 inhibitors and GLP1 analogues, there is one substance each that can also be used in patients requiring dialysis, since the substances are degraded elsewhere: Trajenta® (linagliptin, [9]) resp. Ozempic® (semaglutide, [10]). Metformin should be taken at GFR <30, SGLT2 inhibitors are contraindicated in impaired renal function and should only be prescribed at GFR>45. Insulin can be used without restriction in renal insufficiency, the speaker said.
Bolus insulin and lifestyle
With regard to bolus insulin, one should be aware that it could mean a reduction in quality of life for patients. An alternative is the use of GLP1. If bolus insulin is needed, modern devices can be offered for glucose monitoring. The FreeStyle Libre Flash [11] is a device that is a button on the upper arm, equipped with a subcutaneous sensor that measures blood glucose over two weeks, which can be read via the smartphone. This means easier monitoring of glucose levels for those affected. For the costs to be covered by health insurance, a basic insulin is usually sufficient. In addition, there are also devices that continuously measure blood glucose and trigger an alarm if the value deviates from the range. The trend in medical technology developments for diabetes therapy is moving in this direction.
Lifestyle measures remain an important component as part of the basic therapy. If you don’t have time to go into details, you can limit yourself to addressing regular meal intake and elementary eating habits, Dr. Meienberg adds. Simply refraining from consuming sugary drinks can have a positive effect on diabetes patients. Patients should understand that type 2 diabetes is often a complication of overweight and obesity. He said it’s more about counseling the patient, knowing that implementing weight loss is difficult. For those who fail to reduce weight despite being massively overweight, bariatric surgery is an option not to be considered only at a BMI of 50, he said. This is a measure mentioned in the guidelines. The aim is always to weigh up the expected benefits against the impending risks. The fact that it is not just a matter of pure weight reduction, but that this also has a positive influence on morbidity, is expressed in the term “metablic surgery,” the speaker said.
Conclusion
The therapeutic focus is no longer only on glycemic control, but nowadays cardiovascular risk, BMI, heart failure and nephropathy are also considered as parameters relevant to the course of the disease. With GLP1 analogs and SGLT2 inhibitors, two substance classes are available that have a proven additional cardiovascular benefit. Metformin is still considered the first-line drug of standard treatment. The new substance classes have the advantage of producing antihypertensive effects without inducing obesity and hypoglycemia. However, there are still some “caveats”: Nausea is a relatively common side effect with GLP1 agonists. DPP4 inhibitors and GLP1 agonists lead to an increase in pancreatic enzymes; these agents are therefore contraindicated after pancreatitis. Candidiasis is a common side effect with SGLT2 inhibitors, and urinary tract infections are somewhat less common. SGLT2 inhibitors also increase glucagon (antagonist of insulin), so the risk of developing ketoacidosis is increased. The key message in this regard is that patients who do poorly on SGLT2 inhibitors should be thought of as having ketoacidosis, although the blood glucose may not be very high at all. If this is suspected, it should be clarified. Individual studies report an increased incidence of bone fractures, but this is rather speculative. One patient group in which he advises caution with the new antidiabetics is patients with PAOD, saying the benefits must be weighed against potential risks. Overall, however, there is much to be said for the use of these new substance classes of oral antidiabetics, the speaker emphasized.
Source: FOMF Basel
Literature:
- Meienberg F: Antidiabetics: Update with case studies, Fabian Meienberg, MD, Kantonsspital Baselland. FOMF Basel, 29.01.2020.
- Zinman B, et al: for the EMPA-REG OUTCOME Investigators: empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med 2015; 373(22): 2117-2128.
- EASD: European Association for the Study of Diabetes, www.easd.org
- ADA: American Diabetes Association, www.diabetes.org
- SGED: Swiss Society of Endocrinology and Diabetes, www.sgedssed.ch
- ESC: European Societry of Cardiology, www.escardio.org
- Victoza®, https://compendium.ch
- Saxenda®, https://compendium.ch
- Trajenta®, https://compendium.ch
- Ozempic®, https://compendium.ch
- FreeStyle Libre Flash Glucose Monitoring System: www.freestylelibre.ch
HAUSARZT PRAXIS 2020; 15(3): 16-18 (published 3/23/20, ahead of print).











