Breast carcinoma is the most common malignant tumor of the mammary gland. In particular, mutations of the BRCA genes significantly increase the risk of disease, which is why genetic testing can be useful.
More than one in five people develop cancer before the age of 70. This disease is the second leading cause of death in Switzerland. According to the Federal Statistical Office, the number of new cancer cases and deaths has increased in recent years. In women, breast cancer ranks first among the most common cancers at 32% and accounts for 18.3% of deaths. Among other things, gene mutations are responsible for the development of breast carcinoma, as Prof. Felix Hilpert, MD, Hamburg, Germany, pointed out. In particular, the BRCA (BReast CAncer) genes BRCA1 and BRCA2 are among the high-risk genes whose mutation causes about half of hereditary breast cancers.
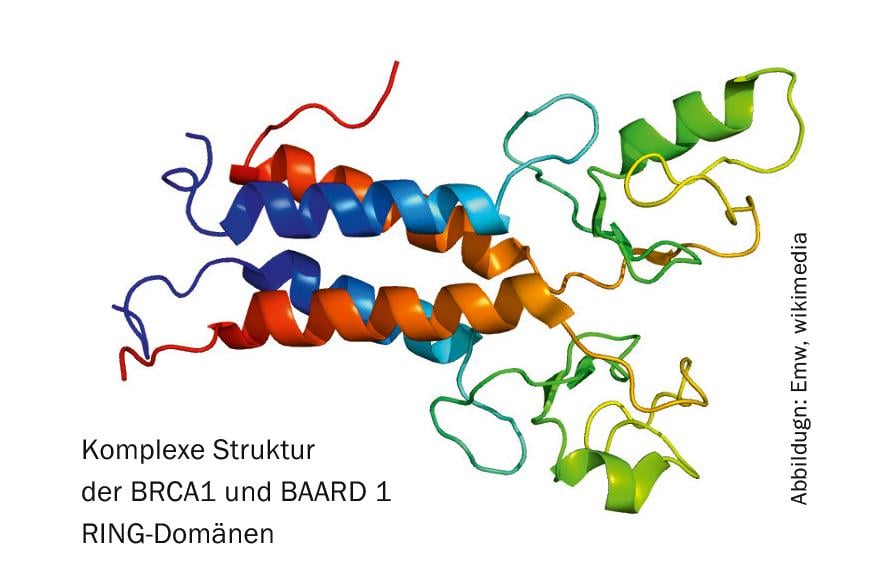
Repair of DNA double-strand breaks
Tumor suppressor genes play an important role in repairing DNA double-strand breaks and thus normally prevent tumor development. If mutations now occur, the uncontrolled proliferation of the defective cells can no longer be prevented. One in 20 patients with breast cancer carries a BRCA mutation. These women usually become ill earlier and often have a less favorable course of the disease. In ovarian cancer, the difficulty lies primarily in the nonspecific symptoms and the lack of established effective early detection options. In a large proportion of those affected (approx. 75%), the disease is diagnosed only at a very late stage, so that curative therapy is often no longer possible.
Especially in the case of familial accumulation, the probability of a BRCA mutation is obvious. With a probability of 50%, the carrier passes on the gene alteration to the next generation. Women and men with high-risk genes for breast cancer have a lifetime risk of developing the disease of up to 80%. In women with BRCA1 mutation, the risk of ovarian cancer is increased to 40% to 60%, and in those with BRCA2 mutation, the risk is increased to 10% to 20%. “Since the therapy setting can be better adapted to the individual situation, diagnostic genetic testing should be considered for the appropriate clientele,” the expert said. In a high-risk family with known BRCA mutations, sonography is recommended every six months and MRI every year starting at age 25 for breast carcinoma, and supplemental mammography at least every two years starting at age 40.
Individual therapy with PARP inhibitors
Olaparib (Lynparza®), an effective PARP inhibitor, is available for therapy. It binds to the active site of poly-ADP-ribose polymerases. This prevents them from dissociating from the DNA and blocks the space for the base excision repair enzymes. A double strand break is the result, which cannot be effectively repaired. The tumor cell becomes unstable. In this way, defects in the DNA repair mechanism are specifically used to cause the cancer cells to die. Currently, the PARP inhibitor is approved in Switzerland for the maintenance treatment of patients with advanced (FIGO stages III and IV) BRCA1/2 mutated (germline and/or somatic) high-grade epithelial ovarian cancer after complete or partial response to first-line platinum-based chemotherapy. In addition, it is indicated as monotherapy in patients with metastatic HER2-negative breast cancer with gBRCA mutation who have been previously treated with anthracycline and a taxane (unless contraindicated) in either a neoadjuvant, adjuvant, or metastatic setting. Patients with hormone receptor (HR)-positive breast cancer should have shown progression under appropriate prior endocrine therapy or be considered unsuitable for endocrine treatment.
Source: Oncology Visit Time, Mutations in Breast and Ovarian Cancer: What Do Women Need to Know?, Sept. 2, 2019, Hamburg (D); MSD SHARP & DOHME/AstraZeneca.
InFo ONCOLOGY & HEMATOLOGY 2019; 7(5): 22.











