Millions of people worldwide suffer from inflammatory bowel disease (IBD) and the prevalence is increasing. To find out more about the role of the microbiome, researchers at Massachusetts General Hospital analyzed data from the gut microbiota of IBD patients and healthy controls. They found that certain strains of gut bacteria are associated with IBD. The results were published in the journal Cell Host & Microbe.
Crohn’s disease (Crohn’s disease) and ulcerative colitis (ulcerative colitis), the two subtypes of IBD, are different on a clinical and molecular level, but both share compelling evidence of a microbiome-based etiology [1,2]. “Inflammation puts tremendous selective pressure on gut bacteria, so we hypothesized that the gut microbiome may contain unique bacterial strains that are associated with inflammatory disease processes in terms of abundance and genetic adaptation,” explained first author Dr. Adarsh Kumbhari, a Research Fellow in Medicine at Massachusetts General Hospital [3]. “To test this hypothesis, we are using evolutionary approaches that can detect bacterial strains in the context of IBD, i.e. Crohn’s disease and ulcerative colitis.” Specifically, this involves the fecal metagenome, which enables large-scale analyses to map bacterial strains that underlie inflammatory processes [1]. Dr. Kumbhari explained that the identification of these bacterial strains can help to uncover which molecular strategies bacteria use to survive during inflammatory processes and to find out more about new microbiome-host interactions that are relevant to disease risk [3].
Multi-stage analysis of stool samples
Based on data sets from 11 studies conducted between 2009 and 2021, the research team extracted stool sample data from 822 IBD patients and 1257 healthy controls, focusing on the genotypes of the bacterial strains [1,3]. They found that hundreds of bacterial strains were more prevalent in stool samples from IBD patients than in healthy controls and that these strains showed long-term evolutionary relationships with the disease. Genomic analysis of these strains revealed key differences in disease-related metabolic pathways, including oxidative stress, biosynthesis of essential nutrients, motility and the bacterial cell wall [1].
In a next step, they analyzed the stool samples of individual IBD patients over time and found that the IBD-associated bacterial strains predominated during periods of high inflammation compared to healthy controls, implying that genetic innovations had given them a survival advantage in the context of IBD [3]. Genetic differences between IBD-associated and health-associated bacterial strains were mapped in relation to known aspects of inflammation – including oxidative stress, nutrient synthesis and immune system invasion.
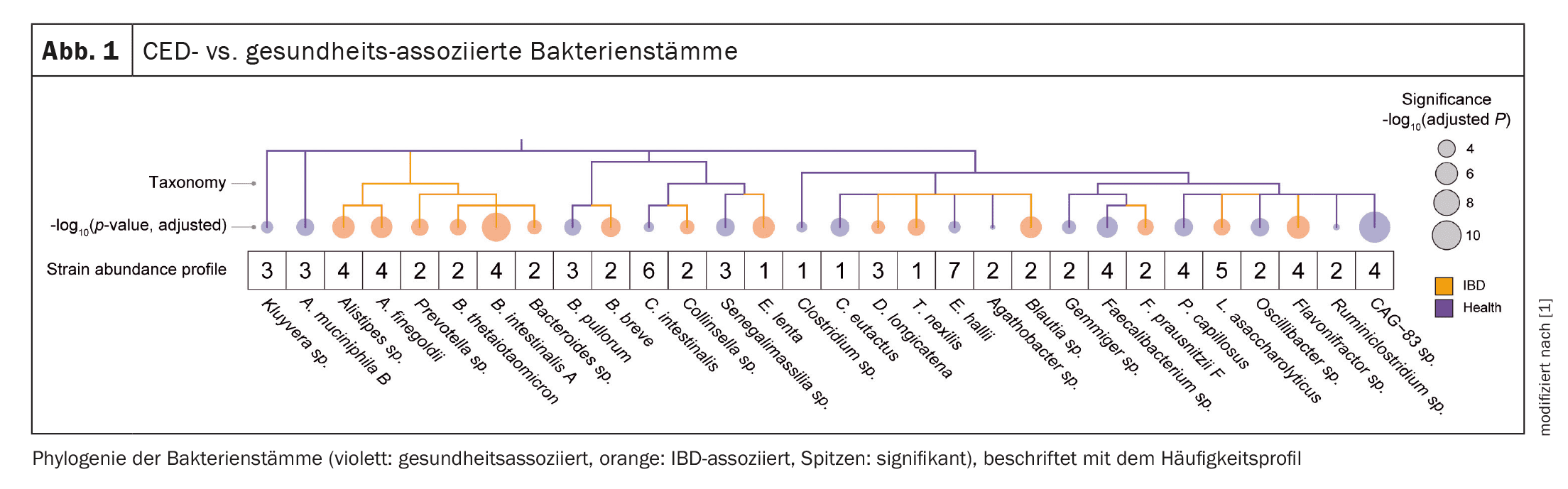
Figure 1 shows an overview of some CED- vs. health-associated bacterial strains that the researchers identified based on prior cluster analysis across different stool samples.
Correlation with fecal calprotectin
Disease-associated strains were also found in healthy individuals, but did not reflect the dominant strain. These could provide colonization resistance, with IBD-associated strains of commensals occupying inflammatory niches to prevent opportunistic colonization by other bacterial invaders [1]. “We also found that the loss of health-associated bacterial strains predicted higher fecal concentrations of calprotectin – a marker of inflammation,” said Dr. Christopher S. Smillie, a senior researcher at the Center for Computational and Integrative Biology at Massachusetts General [3]. “Our findings may have diagnostic utility and the potential to contribute to the development of targeted interventions for IBD and other immune-mediated diseases,” the expert explained [1].
Literature:
- Kumbhari A, et al.: Discovery of disease-adapted bacterial lineages in inflammatory bowel diseases. Cell Host & Microbe 2024; Volume 32: 1147–1162.
- Schirmer M, et al.: Microbial genes and pathways in inflammatory bowel disease. Nat Rev Microbiol 2019; 17: 497–511.
- «Research Identifies Gut Bacterial Strains Linked To Inflammatory Bowel Disease», Massachusetts General Hospital, 24.06.2024.
HAUSARZT PRAXIS 2024; 19(11): 30