Incidence rates of white skin cancer are increasing and timely diagnosis increases the chances of successful treatment. The current s2k guidelines define criteria for grading tumors at high vs. low risk of recurrence and a treatment algorithm based on these criteria.
About 90% of all skin carcinomas are non-melanocytic, making it the most common type of skin tumor. As part of the virtual dermatology and allergology refresher, Martina Ulrich, MD, dermatologist in private practice, Berlin (D), gave an up-to-date overview of the diagnosis and treatment of basal cell carcinoma (basal cell carcinoma, BCC) [1].
Distinguish aggressive from non-aggressive tumors
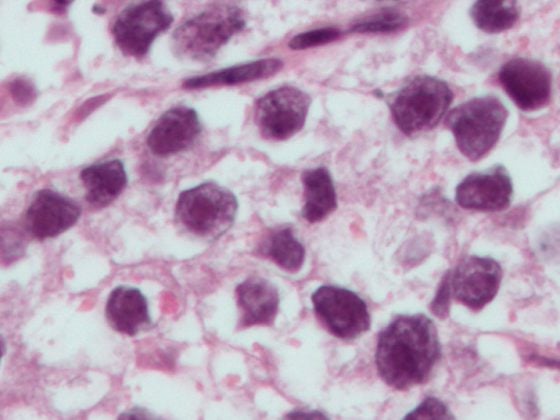
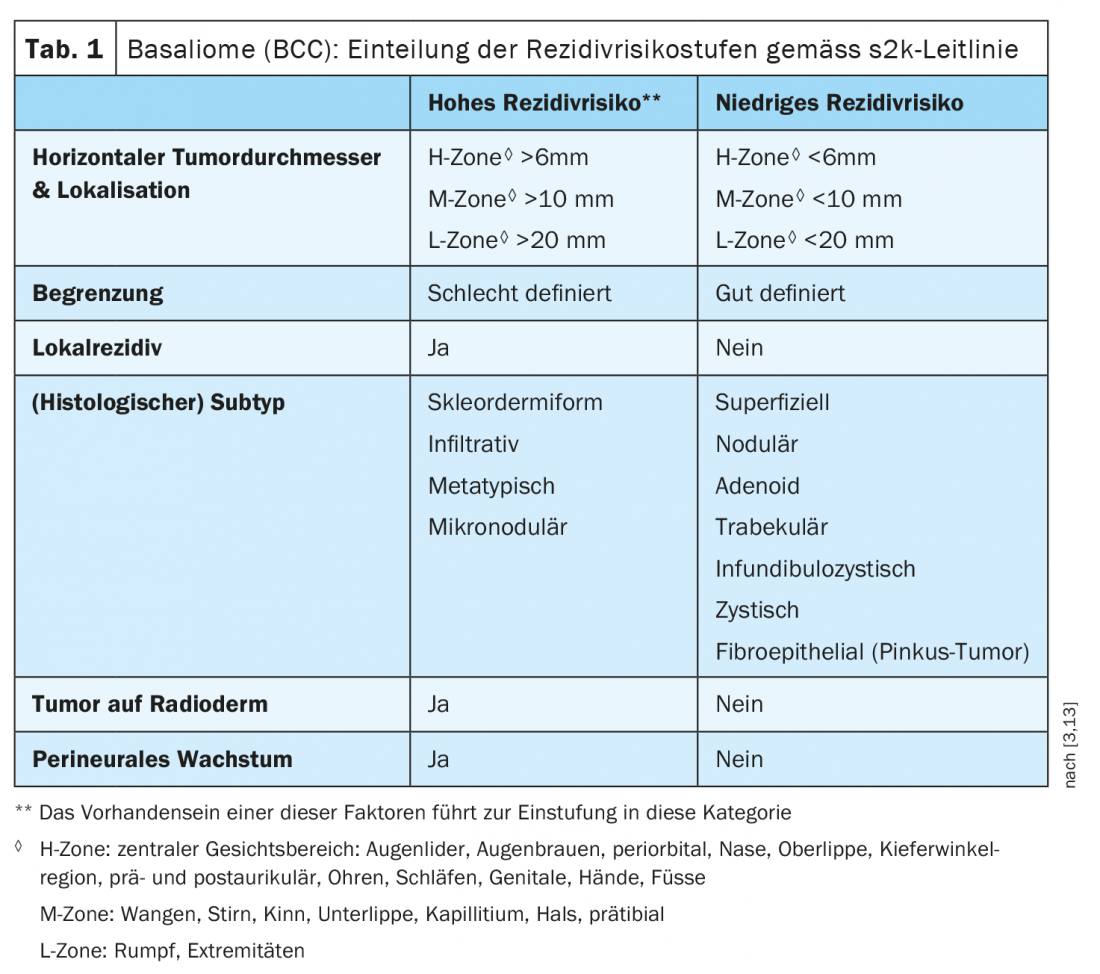
About 65% of all white skin tumors are basaliomas [2]. With very rare exceptions, BCC are non-metastatic but locally infiltrative and destructive, which is why these tumors are sometimes referred to as semimalignant. 90% of basal cell carcinomas occur in sun-exposed areas of the head and neck. In the current S2k-guideline basal cell carcinoma of the skin [3] a distinction is made between aggressive and non-aggressive basal cell carcinoma, which is very important for the therapy, emphasized the lecturer. Aggressive tumors have a significantly higher risk of recurrence (Table 1) . “Non-aggressive basal cell carcinomas are defined as tumors with a diameter of less than 6 mm in high-risk areas, less than 10 mm in other areas of the head and neck, and less than 20 mm in all other parts of the body,” explains Dr. Ulrich [1]. Another criterion relates to the histological findings: the thickness should not exceed 2 mm. “Aggressive tumors are those greater than 6 mm in diameter in high-risk areas and greater than 10 mm in other areas of the head and neck and greater than 20 mm in other parts of the body, as well as all tumors that are sclerosing or morphiphoric or mixed, and also micronodular and basal granular tumors and perinormal invasion.” The treatment algorithm is based on the differentiation between low and high risk of recurrence and is shown in Figure 1. Only in cases of low risk of recurrence (non-aggressive tumors) is tumor thickness a differentiating criterion for the type of therapy. “If this is less than 2 mm, in addition to excision, you can do non-invasive therapy,” she said. These include photodynamic therapy (PDT), imiquimod, 5-FU, local-destructive procedures. If the thickness exceeds 2 mm, surgical intervention should be performed (incision margin-controlled excision or excision with 3-5 mm safety margin). If surgery is not possible, radiatio may be performed. All tumors that have a high risk of recurrence should be operated on according to the guideline. Only if this is not possible or surgery is not desired, or metastasis is present, should an interdisciplinary decision be found in the tumor board. Treatment alternatives include radiation therapy as well as “hedgehog” inhibitors or, more recently, immune checkpoint inhibitors. “For us in practice, this means that we must educate our patients that surgical excision is the first-line therapy for patients and carries the lowest risk of recurrence, and that only depending on other factors can a decision be made to proceed with non-surgical therapy.” One can perform such an operation both micrographically controlled with marginal incision control or with safety distance and in superficial variants the so-called “shave” excision is also mentioned as an alternative.

Which tumors can be treated with PDT?
Many patients have a need for nonsurgical treatments, the speaker said. It is important to properly grade tumors and educate patients that alternatives to surgery are possible when the risk of recurrence is low and tumor thickness is ≤2 mm, he said. On the one hand, there is photodynamic therapy (PDT), which in Germany and Switzerland can be performed as ALA-PDT with aminolevulinic acid (Ameluz®) or as MAL-PDT methylaminolevulinate (Metvix®). Whereby only the conventional form of PDT is approved, i.e. with lamp irradiation in the wavelength range around 635 nm (=red light) [3]. There is a relatively large evidence base for this form of therapy. Multiple randomized trials of the use of PDT for basal cell carcinoma have reported a cure rate of 92% to 97% with MAL-PDT, with a recurrence rate of 9% at one year [4,5]. Using ALA-PDT, healing rates of up to 89% have been achieved [6]. Localization of basal cell carcinoma in the head and neck region and tumor size of >10 mm were identified as negative predictors of recurrence rate in a retrospective case series and cohort study of 323 patients [7]. For nodular BCC, MAL-PDT can achieve cure rates of 91%, with 76% of patients still tumor-free after 5 years [3]. However, in direct comparison, PDT was inferior to surgical excision in terms of recurrence rates (14% vs. 4% recurrence rate at 5 years) [8,9]. In another study, localization to the extremities was found to be a negative response predictor of MAL-PDT [10]. According to a 2016 meta-analysis that included 596 nodular BCC from 5 randomized-controlled trials, after performing MAL-PDT, the rate for tumor freedom was 79% at 5 years [11]. According to the s2k guideline, preparatory removal of crusts is of particular importance for the therapy of nodular basal cell carcinoma and is therefore recommended [12]. From a methodological point of view, it is pointed out that in most of the studies the tumor thickness (penetration depth) is not taken into account, but this has a relevance for the risk of recurrence especially in nodular basal cell carcinoma.
With PDT, two sessions should be performed at a time, preferably 1 week apart, with follow-up 3 months later, Dr. Ulrich explains. If it appears that not everything has healed, another treatment may be given, again two sessions 1 week apart. Only then can one definitively assess whether the lesion has healed or not.
Imiquimod and 5-FU as proven topical treatment alternatives.
Furthermore, imiquimod 5% (Aldara®) is approved for non-surgical therapy and can be used for superficial basal cell carcinoma. Again, this treatment alternative can be used mainly in contraindications regarding surgery, in a treatment frequency of five times a week for a period of 6 weeks, with two days off. Healing rates are very good, the speaker explained, over 80% after three years and sustained high until after five years. However, the side effects can become noticeable over a relatively long period of time.
Also 5-fluorouracil (5-FU) as a topical externum (Efudix®) is a well-tried drug for the non-surgical therapy of basal cell carcinoma. Unlike imiquimod, it does not cause flu-like symptoms. However, the rate for tumor freedom at 12 months was about 70% at 3 years, significantly lower than with imiquimod and with PDT, she said. The recommended frequency of treatment: twice a day for 4 weeks.
In elderly patients, for example in nursing homes, who have far advanced, rarely also metastasizing basal cell carcinoma, one should consider whether there is an alternative possibility to treat with “hedgehog” inhibitors or also to irradiate.
Follow-up and nicotinamide for relapse prophylaxis
The previous recommendation of once-a-year follow-up to rule out local recurrence has been changed to every six months, Dr. Ulrich said. In cases of high risk of recurrence, follow-up is recommended every three months for a period of two years, and thereafter also once a year. Many patients want advice on recurrence prevention. In this context, the prescription of nicotinamide may be useful. The guideline recommends nicotinamide 500 mg twice daily as secondary prevention in patients with a history of basal cell carcinoma. This substance showed a preventive effect with regard to basal cell carcinoma (BCC), spinalioma (SCC) and actinic keratosis. The use of retinoids, on the other hand, is not recommended.
Source: FomF (D) Dermatology and Allergy 2020
Literature:
- Ulrich M: White skin cancer: what to use, in whom? Martina Ulrich, MD. Dermatology and Allergology Refresher, Hofheim (D), 11.09.2020.
- Teske S, Beise U: Skin tumors, Medix, last revised: 12/2019, last modified: 12/2019, www.medix.ch
- AWMF: S2k-Leitlinie Basal cell carcinoma of the skin – Part 1: Epidemiology, genetics and diagnostics, www.awmf.org/uploads/tx_szleitlinien/032-021l_S2k_Basalzellkarzinom-der-Haut_2018-09_01.pdf
- Basset-Seguin N, et al: Topical methyl aminolaevulinate photodynamic therapy versus cryotherapy for superficial basal cell carcinoma: a 5 year randomized trial. Eur J Dermatol 2008; 18: 547-553.
- Szeimies RM, Ibbotson S, Murrell DF: A clinical study comparing methyl aminolevulinate photodynamic therapy and surgery in small superficial basal cell carcinoma (8-20 mm), with a 12-month follow-up. JEADV 2008; 22: 1302-1311.
- Peng Q, et al: 5-Aminolevulinic acid-based photodynamic therapy. Clinical research and future challenges. Cancer 1997; 79: 2282-2308 S2k guideline 032-021 “Basal cell carcinoma” (update 2017/18) 67
- Kessels J, et al: Two-fold illumination in topical 5-aminolevulinic acid (ALA)-mediated photodynamic therapy (PDT) for superficial basal cell carcinoma (sBZK): A retrospective case series and cohort study. J Am Acad Dermatol 2016; 74(5): 899-906.
- Rhodes LE, et al: Photodynamic therapy using topical methyl aminolevulinate vs surgery for nodular basal cell carcinoma: results of a multicenter randomized prospective trial. Arch Dermatol 2004; 140: 17-23
- Rhodes LE, et al: Five-year follow-up of a randomized prospective trial of topical methyl aminolevulinate-photodynamic therapy versus surgery for nodular basal cell carcinoma. Arch Dermatol 2007; 143: 1131-1136.
- Fantini F, et al: Photodynamic therapy for basal cell carcinoma: clinical and pathological determinants of response. JEADV 2011; 25: 896-901.
- Zou Y, et al: Photodynamic therapy versus surgical excision to basal cell carcinoma: meta-analysis. Journal of Cosmetic Dermatology 2016; 15, 374-382.
- Kuijpers D, et al: Similar effectiveness of methyl aminolevulinate and 5-aminolevulinate in topical photodynamic therapy for nodular basal cell carcinoma. J Drugs Dermatol 2006; 5: 642-645.
- NCCN Clinical Practice Guidelines in Oncology: Basal Cell Skin Cancer, J Natl Compr Canc Netw 2016; 14: 574-597.
DERMATOLOGIE PRAXIS 2020; 30(6): 48-50 (published 12/6/20, ahead of print).