In the case of injuries and infections in the brain, the surrounding glial cells ensure that the sensitive nerve cells are preserved and that rampant nerve damage is prevented. A research team at Charité – Universitätsmedizin Berlin has now been able to show how important the reorganization of scaffold and membrane structures in the glial cells is in this process. The findings, now described in the journal Nature Communications*, shed light on a new cellular protective mechanism through which the brain could actively counteract severe courses of neurological diseases.
The nervous system is particularly sensitive to damage, since nerve cells that have died cannot be renewed. Therefore, especially in the brain, different cells have to work together in a coordinated way to limit the damage after injuries and infections, for example, and to enable healing. So-called astrocytes, the most abundant glial cells in the central nervous system, take a central role in protecting the surrounding tissue. Its protective program – called reactive astrogliosis – supports scar formation, helping to prevent the spread of inflammation and limit tissue damage. At the same time, astrocytes can ensure the survival of neurons in close proximity to tissue injury and support the realignment of neuronal networks. Scientists at the Charité have now elucidated a new mechanism of how these processes take place and are coordinated in astrocytes.
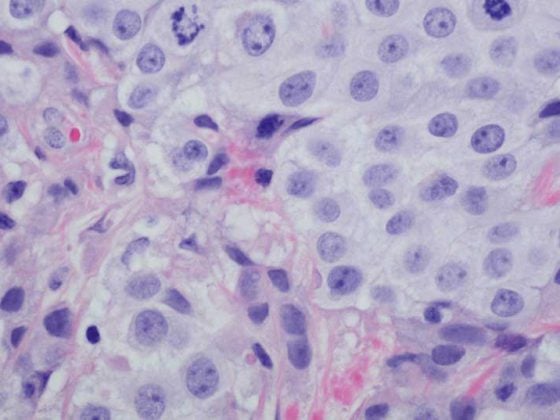
“We were able to show for the first time that the protein drebrin controls astrogliosis in brain injuries,” says Prof. Dr. Britta Eickholt, director of the Institute of Biochemistry and Molecular Biology at Charité and head of the study. “Drebrin is required for astrocytes to form scars as a collective and protect surrounding tissue.” The researchers were able to knock out drebrin in astrocytes – and recreate its role in brain injury in animal models. They studied the cellular changes using electron microscopy and high-resolution light microscopy on the brain – as well as in real time on isolated astrocytes in cell culture. “Loss of drebrin leads to suppression of normal astrocyte activation,” explains Prof. Eickholt. “On the contrary, instead of responding protectively, these astrocytes actually lose their function entirely and give up their cellular identity.” Injuries that are actually harmless thus spread without the protective scarring and more and more nerve cells die.
To enable this scarring, Drebrin controls the reorganization of the actin cytoskeleton, a scaffold for mechanical stabilization, in astrocytes. In this way, the formation of long membrane tubes – so-called tubular endosomes – is also influenced, which serve for the uptake, sorting and redistribution of surface receptors and are necessary for the protective countermeasures of the astrocytes. “Our findings thus show how drebrin controls fundamental functions of astrocytes in defending against harmful influences via the dynamically changing cytoskeleton and membrane structures,” summarizes Prof. Eickholt. “In particular, the membrane tubes that are formed in this process have not been described in this form before in cultured astrocytes or in the brain.”
“Its role as a regulator of the cytoskeleton suggests that drebrin may be a potential risk factor for severe courses of neurological as well as other diseases, because loss of the protein in astrocytes can cause very similar changes,” adds Prof. Eickholt. “It is also possible that affected individuals with Drebrin gene defects – comparable to the animal model – are completely unremarkable until cellular stress, environmental toxins, or disease trigger their expression.” Studies on samples from patients will now clarify the extent to which drebrin also plays a role in other diseases, such as Alzheimer’s disease.
*Schiweck J et al. Drebrin controls scar formation and astrocyte reactivity upon traumatic brain injury by regulating membrane trafficking. Nat Commun (2021), doi: 10.1038/s41467-021-21662-x.
Original publication:
https://www.nature.com/articles/s41467-021-21662-x