Differences in mental health outcomes in diabetic patients with concomitant severe mental illness are often associated, at least in part, with suboptimal cardiovascular risk monitoring. A Dutch-Scottish research group investigated whether these outcomes could be due to inequalities in the translation of cardiovascular monitoring into appropriate risk management depending on SMI status.
In diabetics, comorbid severe mental illness (SMI) is associated with a higher risk of cardiovascular disease. However, there is little research on how target levels of cardiovascular risk factors differ according to SMI status. Previous studies on SMI and cardiovascular risk management in people with diabetes have focused on examining lipid levels, blood pressure and/or blood glucose levels, as these important cardiovascular risk factors can be treated pharmacologically if lifestyle modification is ineffective.
The results were contradictory: some studies found no difference in risk factors, while others found either better or worse lipid levels, better blood pressure and better or worse blood glucose management in people with SMI. In addition, most studies did not distinguish between the different types of SMI. A research group from The Hague and Edinburgh led by Jonne G. ter Braake, Department of Public Health and Primary Care, Leiden University Medical Centre, The Hague, addressed these limitations by comparing the achievement of lipid, blood pressure and blood glucose goals one year after diagnosis of type 2 diabetes by SMI status using a national cohort study in Scotland [1]. In secondary analyses, the researchers also examined statin prescribing by SMI status.
Cholesterol, blood pressure and HbA1c as reference values
The researchers conducted a retrospective cohort study of adults diagnosed with type 2 diabetes in Scotland between 2004 and 2020 and determined SMI status using hospital admission data. They compared total cholesterol levels, systolic blood pressure and HbA1c target levels one year after diabetes diagnosis, as well as statin prescription at the time of diagnosis and one year after.
The study included 291 644 people diagnosed with type 2 diabetes, of whom 3024 (1.0%), 1400 (0.5%) and 9721 (3.3%) had a previous hospitalization for schizophrenia, bipolar disorder and major depression, respectively. Overall, the cohort included more men (56.9%) than women, although women were slightly overrepresented in the groups with previous major depression and bipolar disorder (59.3% and 59.1%, respectively). Compared to those without SMI, those with such a condition at the time of diabetes diagnosis were younger and more likely to live in deprived areas, have a history of alcohol dependence and active smoking status. At the time of diabetes diagnosis, mean BMI and mean total cholesterol levels were slightly higher and mean blood pressure lower in people with SMI than in those without SMI. Patients with depression and bipolar disorder (but not schizophrenia) were more likely to have a history of cardiovascular disease and other comorbidities than those without mental illness. HbA1c levels at the time of diabetes diagnosis were similar in all groups.
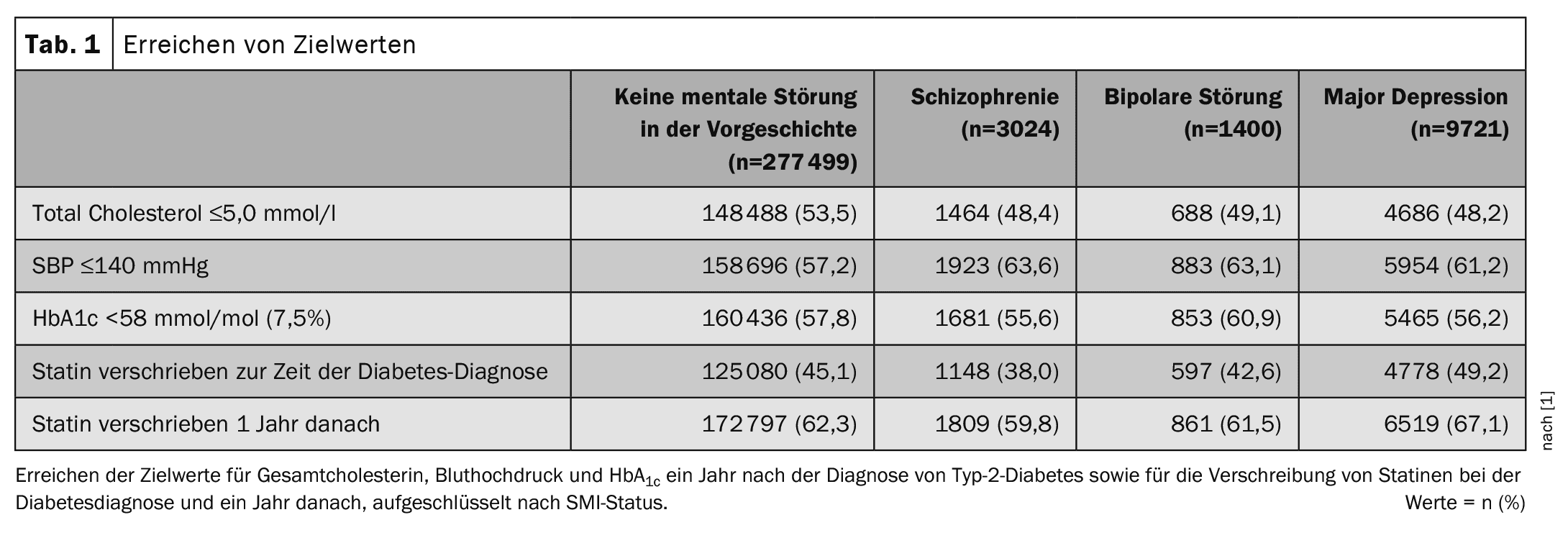
In the entire cohort, 53.5%, 57.2% and 57.8% of individuals achieved the target values for total cholesterol (≤5.0 mmol/l), systolic blood pressure (SBP, ≤140 mmHg) and HbA1c (<58 mmol/mol, 7.5%), respectively. Compared to patients without mental illness, fewer people with each SMI achieved the target values for cholesterol levels. In contrast, a higher proportion of people with SMI achieved the SBP target values (Table 1).
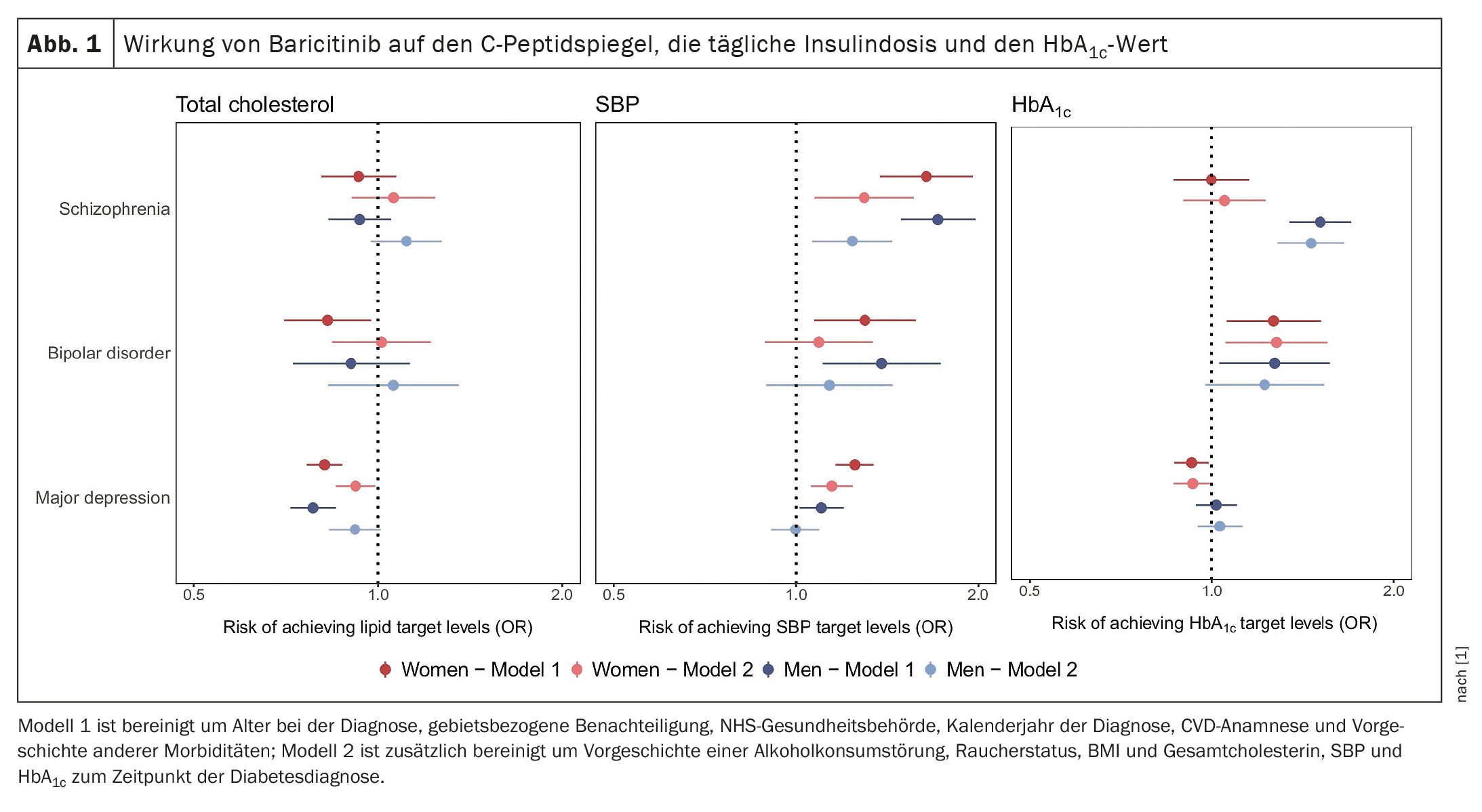
In the model adjusted for sociodemographic factors and clinical history, women with bipolar disorder (odds ratio, OR, 0.83; 95% CI 0.70–0.97) and individuals with major depression (men: OR 0.78; 95% CI 0.71–0.85; women: OR 0.82; 95% CI 0.77–0.87) were less likely to reach target cholesterol levels than individuals without a history of mental illness. There was no statistically significant difference in patients with schizophrenia or men with bipolar disorder (Fig. 1). The inclusion of lifestyle-related factors in the model weakened the association between SMI status and achievement of the cholesterol target value.
SMI sufferers are more likely to achieve blood pressure targets
Interestingly, people with SMI were more likely to reach blood pressure targets than people without mental illness, the authors write. The effect estimates were statistically significant for all SMI disorders, with the magnitude of the effect being greatest for schizophrenia (men: OR 1.72; 95% CI 1.49–1.98; women: OR 1.64; 95% CI 1.38–1.96). Again, the estimates were attenuated after adding lifestyle-related factors (Fig. 1), but remained statistically significant for men and women with schizophrenia and women with major depression.
In people with schizophrenia, the likelihood of reaching the HbA1c target differed by gender: compared to people without mental illness, men with schizophrenia were more likely to reach the value (OR 1.51; 95% CI 1.34–1.70), but there was no difference in women. Both men and women with bipolar disorder were more likely to reach the HbA1c target than the comparison groups (men: OR 1.27; 95% CI 1.03–1.57; women: OR 1.27; 95% CI 1.06–1.51). For people with major depression, there was no difference in the odds in men, but a slightly lower odds in women (OR 0.93; 95% CI 0.87–0.99). The effect estimates were very similar after lifestyle-related factors were added to the models, the researchers said.
More statins are prescribed for depression
At the time of diabetes diagnosis, 45.1% of the cohort received a statin prescription. This proportion increased to 62.4% 1 year later. The proportion of statin prescriptions was highest in people with major depression both at the time of diabetes diagnosis and one year later, followed by people with no history of mental illness. Patients with schizophrenia and bipolar disorder were less likely to be prescribed a statin.
In diabetes patients with no history of cardiovascular disease (CVD) at the time of diagnosis, people with schizophrenia and bipolar disorder were similarly likely to be prescribed statins for the primary prevention of CVD as those without mental illness. However, people with major depression were more likely to be prescribed statins than those without a history of mental illness (OR 1.14; 95% CI 1.08–1.19). However, people with a history of CVD were less likely to be prescribed statins than those without mental illness (schizophrenia: OR 0.54; 95% CI 0.43–0.68; bipolar disorder: OR 0.75; 95% CI 0.56–1.01; major depression: OR 0.92; 95% CI 0.83–1.01). Further adjustment for additional variables, including lifestyle-related factors, resulted in similar or attenuated estimates (Fig. 2).
At one year after diabetes diagnosis, those with SMI were more likely to be prescribed a statin than those without a history of CVD. Among those with a history of CVD, the likelihood of statin prescription was lower in those with schizophrenia and bipolar disorder, whereas there was no clear difference in those with depression, ter Braake and colleagues conclude (Fig. 2).
The results showed that people with SMI were not only equally or more likely to receive routine diabetes monitoring (in primary care), but were also equally or more likely overall to achieve blood pressure and HbA1c targets, but not necessarily cholesterol targets, in the short term after diabetes diagnosis. According to the authors, this underscores the importance of examining these associations with individual SMI impairment and gender, as it provides new insights into how the relationship between SMI and achievement of cardiovascular risk factor targets may vary according to these factors. An example of this is the fact that women, but not men, with major depression are slightly less likely to reach HbA1c targets within the first year of diabetes diagnosis. As the available data in this area is so far limited, further studies would need to investigate this finding in other populations and settings to confirm or refute the patterns.
The association between SMI status and statin prescribing differed according to history of CVD. These results show a worrying inequality in this high-risk subgroup with complex needs. It highlights the importance of a clinical review of statin prescribing, particularly for secondary prevention of CVD in people with SMI, the authors said. Further research to identify the reasons for these inequalities is needed to develop appropriate interventions, they added.
Take-Home-Messages
- SMI were associated with a higher or lower probability of achieving blood pressure and cholesterol targets.
- The results for HbA1c varied according to gender and mental disorder.
- SMI was associated with a lower likelihood of statin prescribing in people with pre-existing CVD.
Literature:
- Ter Braake JG, Fleetwood KJ, Vos RC, et al: Cardiovascular risk management among individuals with type 2 diabetes and severe mental illness: a cohort study.Diabetologia 2024; 67: 1029-1039; doi: 10.1007/s00125-024-06111-w.
InFo DIABETOLOGIE & ENDOKRINOLOGIE 2024; 1(3): 34–37