An important message from the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) is that patients with psoriatic arthritis (PsA) should be treated on an individualized basis according to phenotype and predominant symptoms. There is a wide range of treatment options available today. A domain-specific approach is recommended in the choice of disease-modifying drugs (DMARDs), taking into account comorbidities as well as various other factors.
About one in three psoriasis patients develops psoriatic arthritis (PsA) during the course of the disease. The diagnostic latency since onset of skin psoriasis averages ten years [1]. The typical age of manifestation of PsA is 35-50 years [2]. Pathophysiologically, cytokine-mediated proinflammatory processes lead to an inflammatory response in the inner layer of the joint capsules, resulting in articular cartilage damage and bone erosion [2]. Therapeutically, a reduction in radiographic progression and inflammation is targeted. Severe joint involvement argues for early use of DMARDs. Thanks to currently available modern treatment options, remission is nowadays an achievable treatment goal in PsA [3].
Criteria-based selection of the appropriate therapeutic option
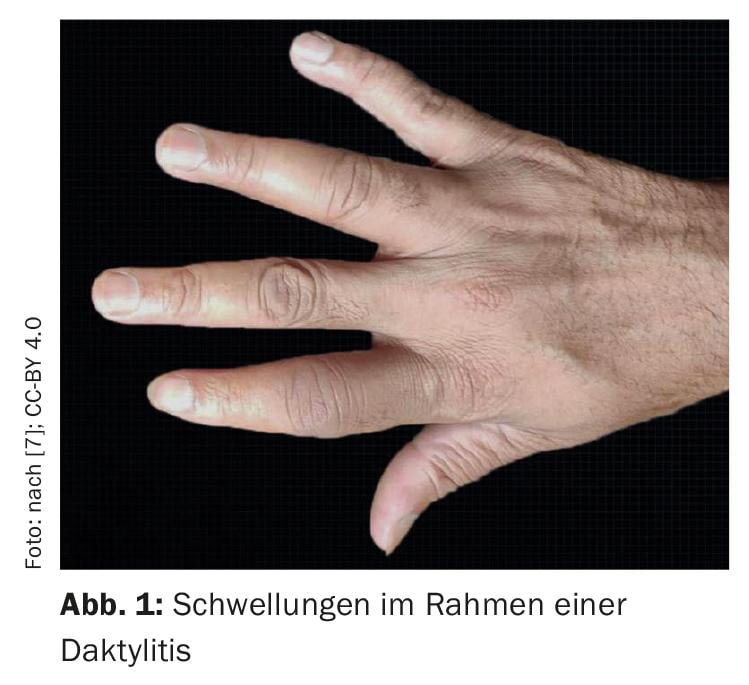
In addition to disease activity and prognostic factors such as structural damage or concomitant diseases, previous therapies, treatment costs, and patient preferences are also decision-relevant criteria [4]. According to a modern understanding of the disease, PsA is considered a multidimensional disease, therefore it is important to consider all domains, i.e. arthritis, enthesitis, dactylitis (Fig. 1), axial involvement, skin and nail involvement. Evidence for the efficacy of different disease-modifying drugs (DMARDs) may vary by disease domain. There is evidence-based efficacy data on this. For its recommendations, the GRAPPA expert group reviewed literature data through August 2020 and reached the following conclusions [4–6]:
- For peripheral arthritis, most available drugs are similarly effective. If conventional DMARDs (csDMARDs) are not sufficiently effective, JAK inhibitors and phosphodiesterase-4 (PDE-4) inhibitors as well as biologics may be considered. There is good evidence for TNF-alpha inhibitors, and the same is true for anti-interleukin (IL)-17, anti-IL-23, and anti-IL-12/23. Non-steroidal anti-inflammatory drugs (NSAIDs) and oral or intra-articular corticosteroids are also mentioned as alternatives for controlling inflammatory processes.
- In PsA patients with axial arthritis, in addition to NSAIDs and physiotherapeutic measures, TNF-alpha inhibitors and IL-17 inhibitors as well as JAK inhibitors have proven particularly effective. With regard to IL-12/23 and IL-23 inhibitors, the GRAPPA experts consider the data situation to be insufficient. The use of csDMARDs is not recommended.
- The best evidence for the treatment of enthesitis and dactylitis is for TNF-alpha inhibitors, as well as all IL-17, IL-23, and IL-12/23 inhibitors.
- In PsA patients with comorbid inflammatory bowel disease (IBD) , preference is given to the use of TNF-alpha inhibitors (except etanercept), IL-12/23 inhibitors, or JAK inhibitors.
- If uveitis is present as a comorbidity , TNF-alpha inhibitors are in first place (with the exception of etanercept).
After therapy goals are achieved: “Consider “tapering
If remission or low disease activity could be achieved, tapering and eventual discontinuation of therapy can be considered according to GRAPPA recommendations [4]. The procedure may vary individually. In addition to reducing the dosage, the treatment intervals can also be extended. The decision to discontinue therapy should be made in close collaboration with the patient. It should be noted that it is currently not possible to predict which patients will successfully complete treatment. In discussions between patient and physician, it should also be discussed that discontinuation of treatment may have disadvantages, in particular reactivation of disease activity. It is not known how cessation of effective therapy affects other aspects, for example, increased risk of cardiovascular disease associated with systemic inflammation.
“Shared Decision Making” as important overriding principle
Overall, the GRAPPA recommendations include seven overarching therapeutic principles for the assessment of PsA and patient management [5,6]. Shared decision making with patients is considered very important. The subjective stress of those affected must also be taken into account. For example, nail involvement is very distressing for many patients [5,6]. While many DMARDs can lead to a reduction in skin psoriasis, it has been shown that for nail psoriasis, the best results are achieved with biologics (IL-17, IL-23, IL-12/23 inhibitors, TNF-alpha inhibitors) as well as PDE-4 inhibitors. Patients should be educated about the advantages and disadvantages of the different treatment options.
Literature:
- Ritchlin CT, Colbert RA, Gladman DD: Psoriatic arthritis. N Engl J Med 2017; 376(10): 957-970.
- Veale DJ, Fearon U: The pathogenesis of psoriatic arthritis. Lancet 2018; 391(10136): 2273-2284.
- Tucker LJ, Ye W, Coates LC: Novel Concepts in Psoriatic Arthritis Management: Can We Treat to Target? Curr Rheumatol Rep 2018; 20(11): 71.
- Coates LC, et al: Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol 2022; 18: 465-479.
- Coates LC, et al: The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) Treatment Recommendations 2021, eEULAR 2021, Abstract OP0229, http://dx.doi.org/10.1136/annrheumdis-2021-eular.4091
- “GRAPPA’s Updated Therapy Recommendations for PsA Management,” 12 Oct 2021, www.rheumaguide.de, (last accessed 18 Aug 2022).
- Pustake M, Vidhale T, Nadgire S: Psoriatic Arthritis With Dactylitis: A Case Report and Concise Review of Treatment Options. Cureus 2021; 13(8): e16966. doi:10.7759/cureus.16966.
DERMATOLOGIE PRAXIS 2022; 32(4): 34











