The topic of vaccination skepticism has become the focus of media and health policy in connection with an increase in measles cases in recent months. In debates about vaccinations, different assessments of benefits and risks clash. What are the current findings on this?
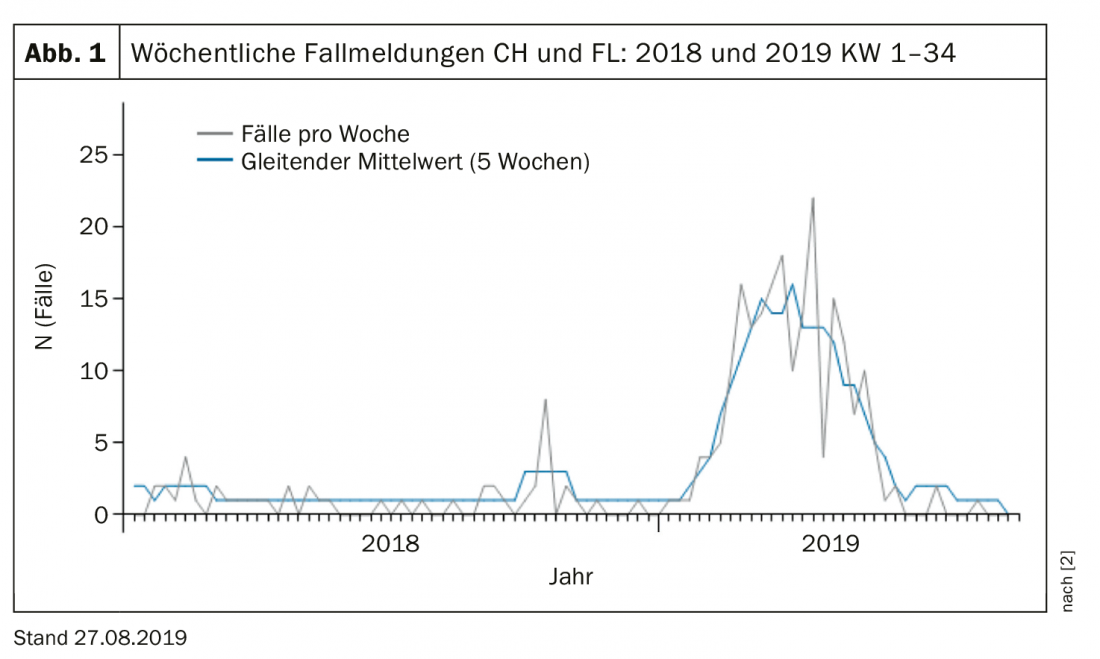
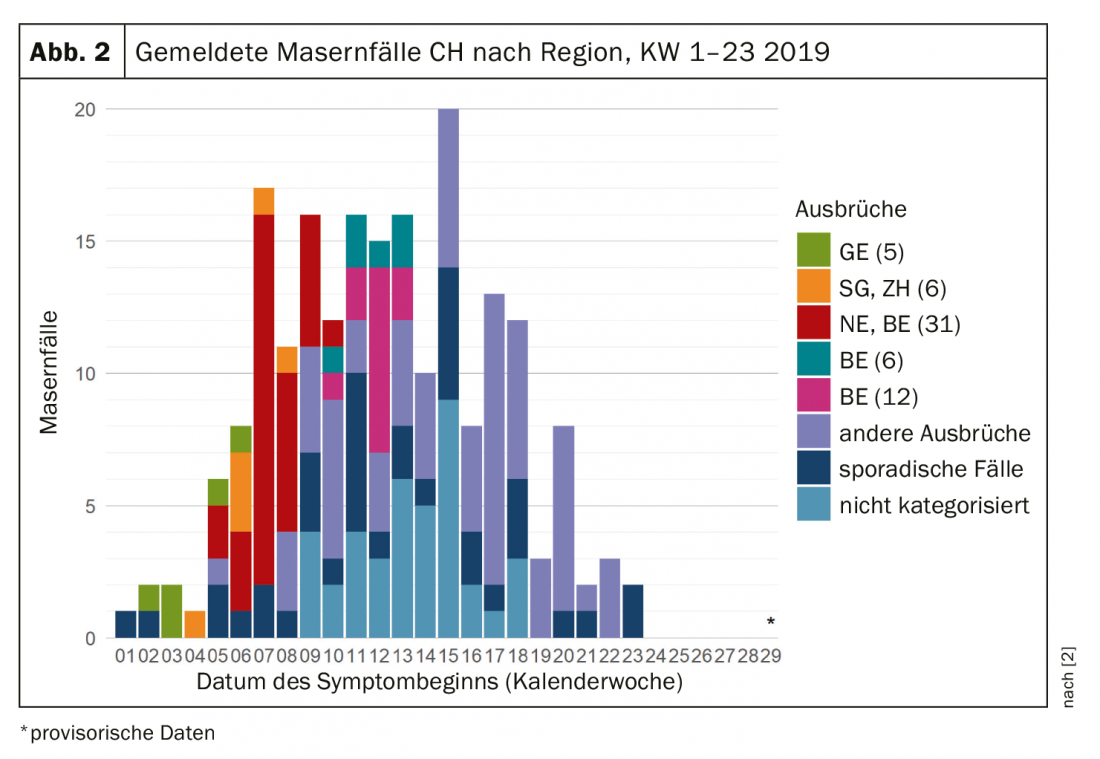
In 2019, more than three times as many measles cases have already been recorded in Switzerland in the first four months of the year as in the whole of 2018 (Figs. 1 and 2) [1,2]. For example, 166 cases of measles were reported in Switzerland from Jan. 1, 2019, to May 6, 2019. In the same period of the previous year, there were only 21 cases. This represents an increase in incidence from 2.5 (2018) to 19.5 (2019) cases per 1,000,000 population [1]. A similar trend is also emerging in other regions. In the first six months of 2018, more than 41,000 children and adults were infected with measles in the WHO European Region, a significant increase compared with the number of cases in previous years [3]. For example, the maximum number of measles cases for the same period between 2010 and 2017 was 23,927 in 2017 and the lowest was 5273 for 2016 [3].
Controversy over mandatory vaccination
In the first half of 2019, two deaths due to measles were reported to the FOPH [1]. According to the FOPH’s estimate, a 95% vaccination coverage rate of children and all adults born after 1963 with two doses would be required to eliminate measles. Unlike Italy and France, where mandatory vaccinations were introduced in 2017/18 to address vaccination skepticism, in Switzerland vaccinations are voluntary. Politically, such a demand would hardly stand a chance in Switzerland, because it would contradict the constitutionally guaranteed freedom of citizens, according to the assessment of experts. In addition, it could be counterproductive by creating a reactance reaction that would have the opposite effect of what was intended by the obligation. According to Prof. Dr. med. Philip Tarr, co-chief physician at the Cantonal Hospital Baselland and head of the National Research Program “Vaccination-Skeptical Parents and Physicians in Switzerland”, a critical attitude towards official recommendations of authorities such as physicians and authorities corresponds to the zeitgeist of a postmodern, individualized society [4]. This understanding of personalized medicine conflicts with the WHO’s goals of eliminating certain diseases, such as measles. Vaccination opponents are therefore classified as a global threat by the WHO [1]. Consequently, unvaccinated persons can endanger other people who have no or no effective vaccination protection (e.g. babies, pregnant women, immunocompromised persons). In this respect, it is a question of weighting individual interests and interests of the common good [1].
How can the vaccination rate be increased?
In Switzerland, measles vaccination rates vary by canton and are 95% in most cantons <and 90% in only a few >[5]. The increase in measles cases is therefore also attributed to insufficient vaccination rates. Vaccine skepticism is not the only reason, because there is also limited access to vaccines in Switzerland. With regard to promoting vaccination coverage, Swiss health policy focuses on improving access to vaccines and communicative aspects [5]. For healthcare professionals, this includes dealing with patients who take a proactive patient role and value a participatory decision-making process, or the situation where parents are overwhelmed with evaluating different and sometimes contradictory information that circulates about vaccination topics. Some parents prefer to consult complementary physicians, although the National Research Program “Vaccine-Skeptical Parents and Physicians in Switzerland” [4] showed that they also provide information about the benefits and risks of vaccination, while increasingly taking into account individual patient needs and fears. This is a different perspective than from an epidemiologic standpoint, but it also has merit and serves an important function in the vaccination debate and care [5]. Thus, the assumption that all complementary physicians are vaccination skeptics or opponents is not justified, and it appears that the level of communication in this setting may be more likely to persuade vaccination-skeptical patients to vaccinate than a health policy mandate or a presentation of epidemiologic facts.
Literature:
- Kohler A: Is the measles situation in Switzerland really that bad? SWI swissinfo.ch, May 14, 2019, www.swissinfo.ch/ger/gesellschaft/masern_ist-die-masern-situation-in-der-schweiz-wirklich-so-schlimm-/44951408
- Federal Office of Public Health: figures on infectious diseases: Measles, www.bag.admin.ch/bag/de/home/zahlen-und-statistiken/
- WHO: Measles reaches peak in European Region, www.euro.who.int/de/media-centre/sections/press-releases/2018/measles-cases-hit-record-high-in-the-european-region, last accessed 02 Sep 2019.
- Swiss National Science Foundation: Health Care: National Research Program. Vaccination-skeptical parents and physicians in Switzerland, www.nfp74.ch/de/projekte/ambulante-versorgung/projekt-tarr
- Tarr PE, Deml MJ, Huber BM: Measles in Switzerland – progress made, but communication challenges lie ahead. Swiss Med Wkly 2019; 149: w20105, https://doi.org/10.4414/smw.2019.20105
- Federal Office of Public Health: Measles – Situation Report Switzerland, www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/masern-lagebericht-schweiz.html
FAMILY PRACTICE 2019; 14(9): 43-44