Depression has come back into the focus of scientific investigation, and not just since the challenges of the Corona pandemic. This is because they are among the most common mental illnesses and can also take a chronic course. This makes effective therapy management based on the latest scientific findings all the more important .
The treatment of depression is usually multimodal with psychotherapy and pharmacological intervention – especially in severe courses. With regard to psychotherapy, it could be shown that all methods can be regarded as equivalent, Prof. Dr. med. Mathias Berger, Freiburg (D), pointed out in his lecture. However, it would take 548 patients in clinical trials for two study arms to even detect significant efficacy differences.
It was concluded that only psychotherapies for which at least ten randomized studies are available should be used in daily practice. In addition, the patient’s wishes and previous experience should be taken into account, and undesirable side effects of each form of psychotherapy should also be considered. “Ultimately, the only undoubted advantage that psychotherapy can claim over pharmacotherapy is sustainability,” the expert said. This is because antidepressants respond much more quickly, but they only work for as long as they are taken, whereas psychotherapy steadily improves symptoms. As a rule, 75% of the effect is achieved after 20 sessions.
Acute treatment with antidepressants
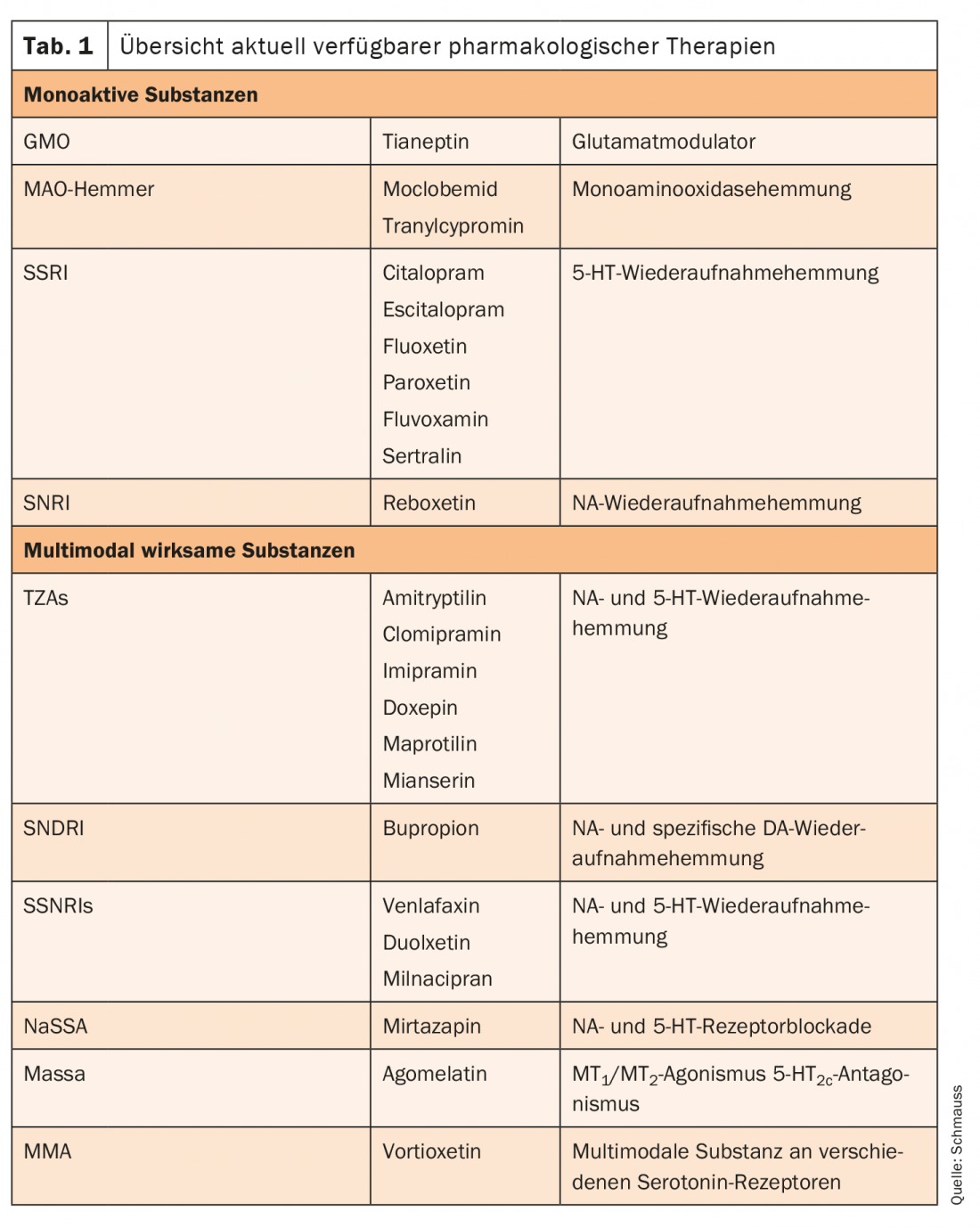
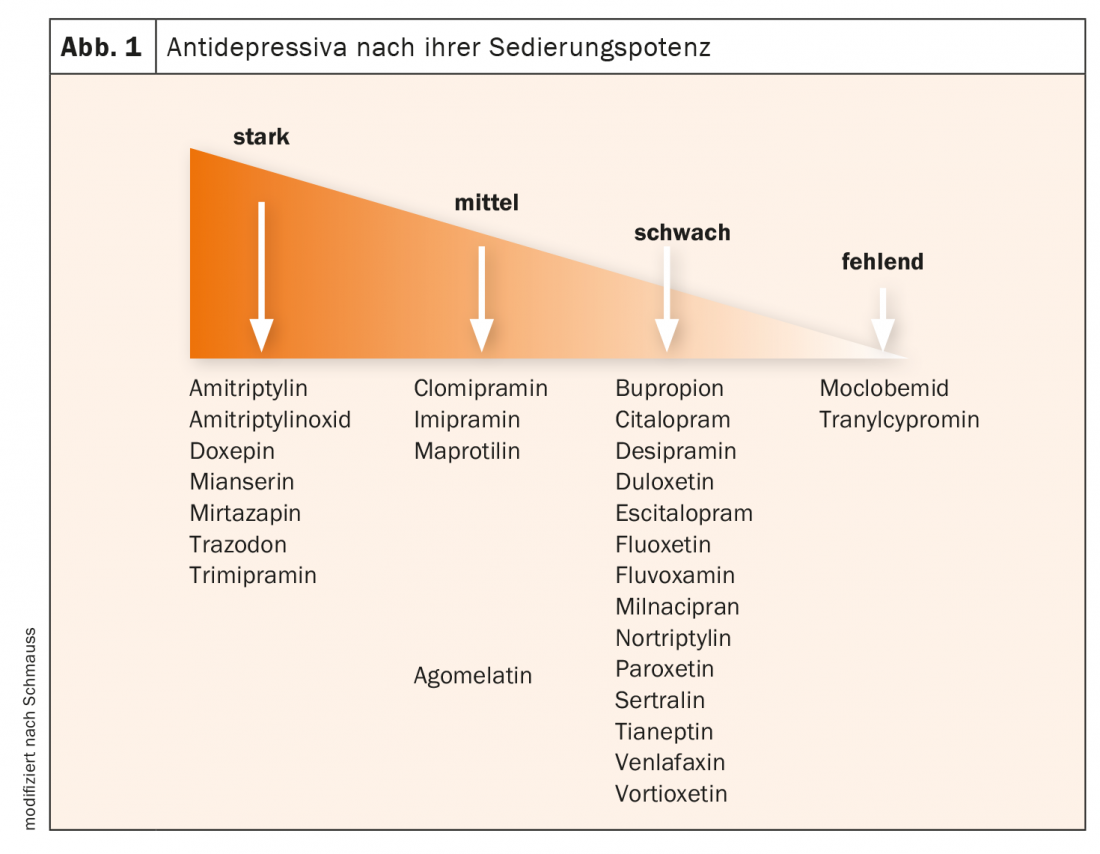
The goal of any treatment is remission, as Prof. Dr. med. Max Schmauss, Augsburg (D), explained. For depression, this corresponds to a HAMD score ≤7. These patients demonstrate improved physical and social functioning and a lower risk of relapse. To achieve this, pharmacological interventions are resorted to, especially in moderate and severe forms – as monotherapy or in combination with psychotherapy. There are currently a number of antidepressants available. Pharmacologically, these can be divided into monoactive substances and dual- or multimodal-acting substances (Table 1) . “Clinically, we tend to distinguish the antidepressants according to their initial sedation potent,” Schmauss further reported. An antidepressant should be selected based on several considerations. For example, the tolerability profiles of SSRIs and TCAs differ significantly. Before especially with TZA, serious complications such as delirium, cardiac problems, or urinary retention are more common. In addition, taking a week’s supply of TZA can be lethal in suicidal patients. Therefore, only small package sizes should be prescribed in the outpatient setting. In addition, response in previous episodes of illness, manageability, and the physician’s experience with use play a role in the selection of the appropriate antidepressant.
Plasma level control in non-responders.
If a patient does not respond to the medication after adequate treatment duration and dose and taking it as directed, the plasma level should be monitored. There are now established recommendations for this. With the exception of SSRIs, high-dose therapy (consistent with the recommendations for use) may then be appropriate.
However, augmentation, switching to another agent, or combination administration with another antidepressant may also be considered. Switching antidepressants is the most common strategy implemented after nonresponse to antidepressant therapy. However, its effectiveness is not well enlivened by studies. Overwhelmingly, it is recommended to also change the substance class when changing antidepressants, the expert said. Substances that may be considered for augmentation include lithium, antipsychotics, thyroid hormones, or dopaminergic agents. For example, lithium augmentation should be performed for at least two weeks until remission. However, if there is no improvement after four weeks, it should be discontinued.
Focus on recurrence prophylaxis
After the first episode of major depression, relapse occurs in 41% of patients after one year. After five years, the figure is already 74%, Schmauss cautioned. Each depressive episode increases the risk for another episode. Discontinuation of treatment further increases this. Therefore, effective maintenance therapy is essential. Here, antidepressants show a convincing and lasting effect, Schmauss summed up.
Source: DGPPN 2020
InFo NEUROLOGY & PSYCHIATRY 2021, 19(1): 24-25 (published 2.2.21, ahead of print).











