A lot has happened in the field of diabetes therapy in recent years. Many new active ingredients have appeared on the market. However, metformin and lifestyle modifications are still considered first-line treatments. After that, therapy planning becomes a bit more difficult. Precise knowledge of the effects and side effects of each substance is necessary to make an individualized decision. A possible approach to therapeutic diversity was highlighted by an event at the SGIM Congress in Basel.
In addition to insulin, the administration of which is never wrong in principle, there are the following agents that are relevant in practice. Prof. Marc Donath, MD, Chief of Endocrinology, Diabetology and Metabolism at the University Hospital Basel, discussed the advantages and disadvantages of the individual substances.
What do the guidelines advise?
Key points of the ADA/EASD guidelines (position paper) on type II diabetes are:
- In any case, glycemic targets and therapies must be individualized. “The diabetic is not just an HbA1c,” is the motto. Young healthy patients tend to require more ambitious HbA1c targets (6-6.5%), whereas in older patients the side effect profile and comorbidities become all the more important and targets are therefore adjusted somewhat (7.5-8%). The goal is to avoid hypoglycemia (as it is cardiovascularly significant).
- The basis of treatment remains lifestyle modifications (weight loss, healthy diet, increased physical activity).
- Metformin is first-line agent (combined with lifestyle).
- After metformin, the data are (still) limited and a clear recommendation is therefore difficult.
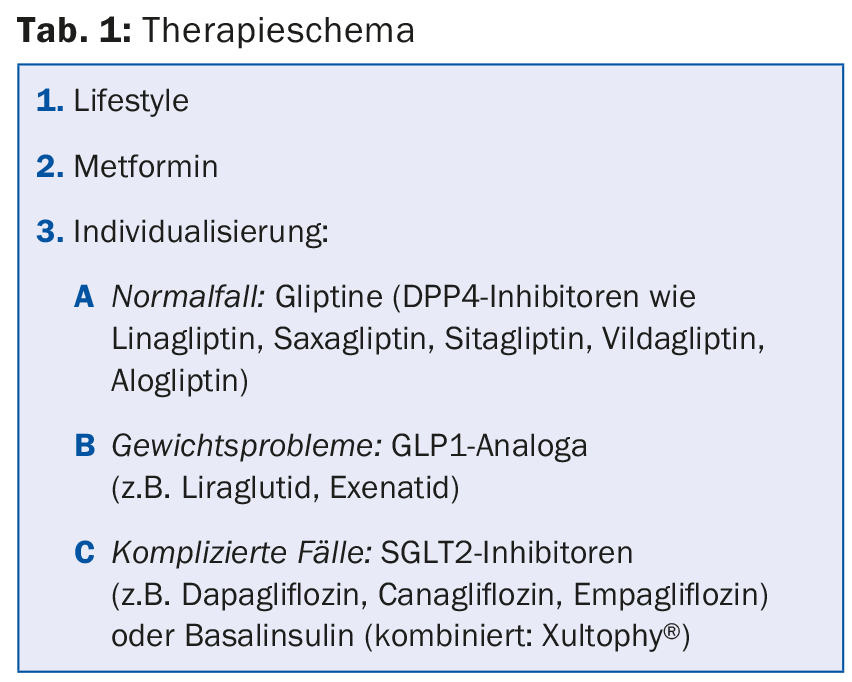
A possible therapeutic regimen is shown in Table 1.
Incretin-based therapies
Incretin-based therapies with DPP-4 inhibitors and GLP-1 receptor agonists are assuming a growing role in diabetes therapy. They are often used in the second-line setting after metformin. Because GLP1 analogues lead to weight loss, they are the primary choice for patients with obesity. Exenatide (Byetta®) is administered twice daily. In the meantime, with Bydureon® there are also a once-weekly form that works very well in about one-third of patients. Among other things, exenatide also slows gastric emptying. The nausea caused by eating too much, which can sometimes occur as a side effect, is almost seen as an effect in terms of weight reduction. However, reduced food intake and body weight loss have also been demonstrated independently of the occurrence of nausea. Liraglutide (Victoza®) is administered once daily. It is also now available as a combination with a basal insulin (insulin degludec), under the name Xultophy®.
SGLT2 inhibitors
SGLT2 inhibitors such as dapagliflozin, canagliflozin, and empagliflozin can generally be combined with all antidiabetic agents. Their effect is insulin-independent. Compared with placebo, they significantly lower HbA1c both in monotherapy and in combination (e.g., with metformin, sulfonylureas, insulin, or DPP4 inhibitors). Blood pressure is also lowered (systolic slightly more than diastolic, about 4-5 mmHg). The decrease is more pronounced in uncontrolled blood pressure. The probability of hypoglycemia is comparable to placebo.
SGLT2 is responsible for approximately 90% of total renal glucose reabsorption. Inhibition of this increases the excretion of glucose in the urine. Plasma glucose is thus reduced, hyperglycemia addressed, and weight loss supported, with 80-100 g glucose = 300-400 cal/d. Weight loss is clinically relevant and lasts for an extended period of time.
Disadvantages include the threat of (uro-)genital infections, which are more likely due to increased glucose excretion in the urine. Summarizing the current study situation, it appears that urinary tract infections are slightly more common compared to placebo. However, while this difference is relatively small and not always present, genital tract infections, on the other hand, occur significantly more often than with placebo.
Also relevant: This is a new class of agents with partially unexplored effects; only recently has it been shown [1] that SGLT2 inhibition drives glucagon secretion. A potentially problematic side effect that needs to be explored in more detail.
“Overall, SGLT2 inhibitors are good drugs, but they have to be used correctly,” Prof. Donath said. “Also, it’s important to remember that we’re only treating the symptoms with this and not the diabetes as such.”
Source: Update Diabetes, SGIM-Congress, May 20-22, 2015, Basel
Literature:
- Bonner C, et al: Inhibition of the glucose transporter SGLT2 with dapagliflozin in pancreatic alpha cells triggers glucagon secretion. Nat Med 2015 May; 21(5): 512-517.
HAUSARZT PRAXIS 2015; 10(7): 45-46











