At the 96th Annual Meeting of the SGDV in Basel, one of the topics was bacterial skin infections. Antibiotics remain first-line treatment options for both erysipelas and furunculosis. Beyond that, however, it is important to reduce the risk of recurrence by addressing predisposing factors as well. Precise knowledge of the pathogenesis is crucial in any case.
(ag) In 1937, the British Medical Journal published the first actively controlled trial of an antibacterial agent (Prontosil®), in the treatment of erysipelas. This was the first synthetic antibiotic to appear on the market. Two years later, Gerhard Domagk was awarded the Nobel Prize for the discovery of the antibacterial effect of sulfonamide. But what is the current diagnostic and therapeutic situation of skin infections such as erysipelas or furunculosis? This was the question addressed by Prof. Dr. med. Stefano Bassetti, Cantonal Hospital Olten, in his lecture at the 96th Annual Meeting of the SGDV.
Erysipelas is defined as an infection of the upper layers of the skin (epidermis, dermis), without an encroachment on subcutaneous tissue. The main cause is β-hemolytic group A (and G) streptococci. Cellulitis, more commonly referred to as phlegmon in German, is an infection that also affects subcutaneous tissue. One possible cause is Staphylococcus aureus. In the USA, the two terms “cellulitis” and “erysipelas” are often used interchangeably.
According to a study [1], in addition to a past erysipelas and a disorder of the cutaneous barrier, for example, a tinea pedis interdigitalis, a chronic leg edema, but also overweight are risk factors for an erysipelas (on the legs). “In addition, the respective susceptibility of a host could have to do with its genetic prerequisites; this is also currently being investigated [2],” the expert said. “Significant risk factors for chronic recurrent forms of erysipelas include skin disease, venous insufficiency, and lymphedema. The latter represented the most prominent risk factor for recurrence [3].”
Antibiotics and more
A recurrent episode is treated with antibiotics like the first one. In addition, tinea pedis interdigitalis should also be addressed and the skin should remain well hydrated (avoid dryness and cracking). Underlying edema, of any type, should be reduced. “Unfortunately, venous ulcers as well as severe lymphedema and high-grade chronic venous insufficiencies require high compression classes when using compression stockings (III-IV), which worsens compliance. As a result, the stockings often end up in the closet, even though they would be so important for preventing new erysipelas recurrences,” says Prof. Bassetti.
Prophylactic antibiotic therapy showed efficacy against recurrence in a recent study [4], but only as long as the antibiotic (penicillin V) was administered. For some well-selected patients, it could be used, the expert said.
Is furunculosis “in” again?
Due to the sharp increase in incidence and hospitalization rates due to S. aureus, boils have come back into increased focus in recent years [5]. But the question is: Why is the incidence increasing in the first place?
- There is a worldwide epidemic of so-called “community associated” MRSA (methicillin-resistant Staphylococcus aureus, CA-MRSA) found outside the disease system.
- There is an association between CA-MRSA and the Panton-Valentine leukocidin (PVL).
CA-MRSA infections manifest primarily in skin and soft tissue, most commonly as boils. The majority of boils in the US are CA-MRSA related, thus the above incidence figures are reflective of this epidemic. In Europe, the prevalences of CA-MRSA in furunculosis are much lower.
PVL, in turn, is a toxin (virulence factor of S. aureus) that can lead to recurrent boils and has a link to necrotizing pneumonia. CA-MRSA are in the majority associated with PVL.
Possible risk factors for CA-MRSA include travel to endemic regions (e.g., the United States) and possibly contact with animals (veterinarians). A recent study [6] among 340 Swiss veterinarians concluded that as many as 3.8% are carriers of nasal MRSA. Consequently, it could be an occupational hazard. “A study from the Lucerne Cantonal Hospital shows: About 23% of MRSA are CA-MRSA,” Prof. Bassetti explained.
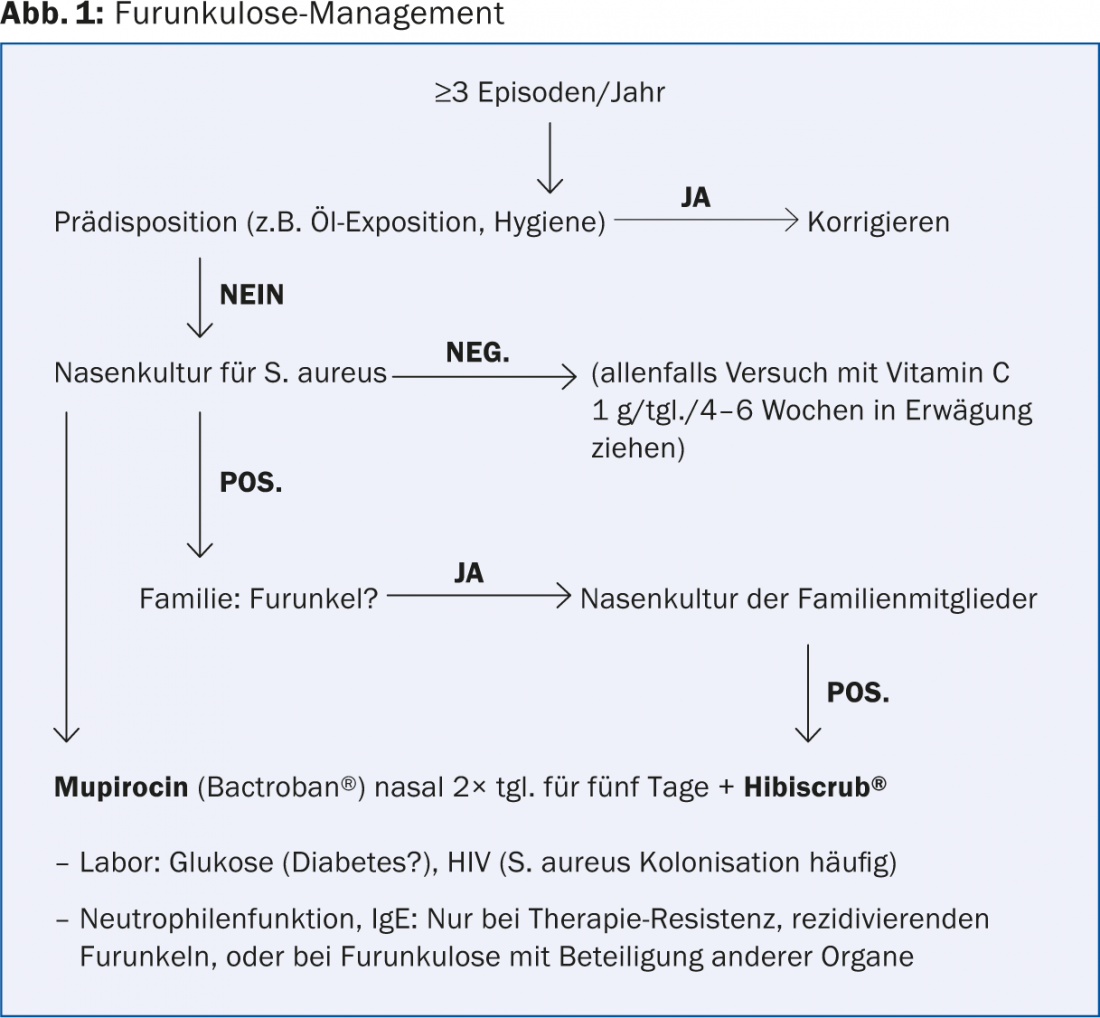
The most important predisposing factor for furunculosis is nasal colonization by S. aureus. Other predisposing diseases include diabetes mellitus, atopic diseases, and rare immunodeficiencies (chronic granulomatosis, Job’s syndrome, Chédiak-Higashi, Wiskott-Aldrich). A possible clarification algorithm for furunculosis is shown in Figure 1.
Source: “Therapy of Chronic Recurrent Pyoderma,” presentation at the 96th Annual Meeting of the SGDV, September 4-6, Basel.
Literature:
- Roujeau JC, et al: Chronic dermatomycoses of the foot as risk factors for acute bacterial cellulitis of the leg: a case-control study. Dermatology 2004; 209(4): 301-307.
- Hannula-Jouppi K, et al: Genetic susceptibility to non-necrotizing erysipelas/cellulitis. PLoS One 2013; 8(2): e56225. doi: 10.1371/journal.pone.0056225. epub 2013 Feb 20.
- Inghammar M, Rasmussen M, Linder A: Recurrent erysipelas – risk factors and clinical presentation. BMC Infect Dis 2014 May 18; 14: 270.
- Thomas KS, et al: Penicillin to prevent recurrent leg cellulitis. N Engl J Med 2013 May 2; 368(18): 1695-1703.
- Suaya JA, et al: Incidence and cost of hospitalizations associated with Staphylococcus aureus skin and soft tissue infections in the United States from 2001 through 2009. BMC Infect Dis 2014 Jun 2; 14: 296.
- Wettstein Rosenkranz, et al: Nasal carriage of methicillin-resistant Staphylococcus aureus (MRSA) among Swiss veterinary health care providers: detection of livestock- and healthcare-associated clones. Schweiz Arch Tierheilkd 2014 Jul; 156(7): 317-325.
DERMATOLOGIE PRAXIS 2014; 24(5): 38-40











