In the largest study of diabetes insipidus to date, more than 1000 patients were enrolled worldwide. The evaluations show that a large proportion of those affected have care deficiencies and many suffer from psychological problems. The results of the online survey were published in Lancet Endocrinology.
Antidiuretic hormone (arginine vasopressin peptide, AVP) is produced in the hypothalamus in the diencephalon and released into the blood by the neurohypophysis. In healthy people, it ensures in the kidney that the body loses as little water as possible. However, this interplay gets out of sync if too much is drunk: those who constantly consume excessive amounts of fluid impair the kidneys’ urine-forming function – they can no longer retain the quantities of fluid [1].
Correctly classify polyuria-polydipsia syndrome
The most common cause of polyuria and polydipsia is the presence of diabetes insipidus centralis, in which the osmosensitive release of AVP (arginine vasopressin peptide) from the neurohypophysis is impaired. Much less common is renal or nephrogenic diabetes insipidus. Here, there is insensitivity of AVP-mediated antidiuresis in the kidneys. The third possible cause is considered to be primary polydipsia. It often results from suppression of AVP release by excessive increased fluid consumption [2].
Large-scale international online survey
The online survey was developed by a team of experts in close collaboration with patient representatives. The direct involvement of people affected by the disease allowed for a strong focus on the study of patient-relevant outcomes. Recruitment for participation in the survey was done through various channels with support from patient organizations. Between 8/23/2021 and 2/7/2022, 1034 patients with central diabetes insipidus participated in the survey [3]. 91% of participants were adults (age range 34-54) and 9% were children and adolescents (age range 6-15). Forty-seven percent of participants had isolated posterior pituitary dysfunction and 53% had combined anterior and posterior pituitary dysfunction. The main causes were idiopathic (30% of cases) or presence of tumors and cysts (46% of cases). 26% of 994 patients receiving desmopressin therapy had hyponatremia leading to hospitalization. In patients in whom desmopressin-an antidiuretic agent in the ADH analgoa group-was routinely omitted or delayed to allow intermittent aquaresis, the prevalence of hyponatremia was significantly lower (OR 0.55; 95% CI: 0.39-0.77; p=0.0006). Of 535 patients hospitalized for any medical reason, 13% (95% CI; 0.10-0.16) did not receive desmopressin without intravenous fluid replacement. Self-reported symptoms of dehydration were present in the patients in question. 64% (n=660) of all participants reported decreased quality of life, and 36% (n=369) reported psychological changes that they perceived to be related to central diabetes insipidus. 80% (n=823) of participants had encountered a situation in which central diabetes insipidus was mistaken for diabetes mellitus by healthcare professionals. 85% of all participants were in favor of renaming the disease. The preferred alternative names were “vasopressin deficiency” and “arginine vasopressin deficiency.”
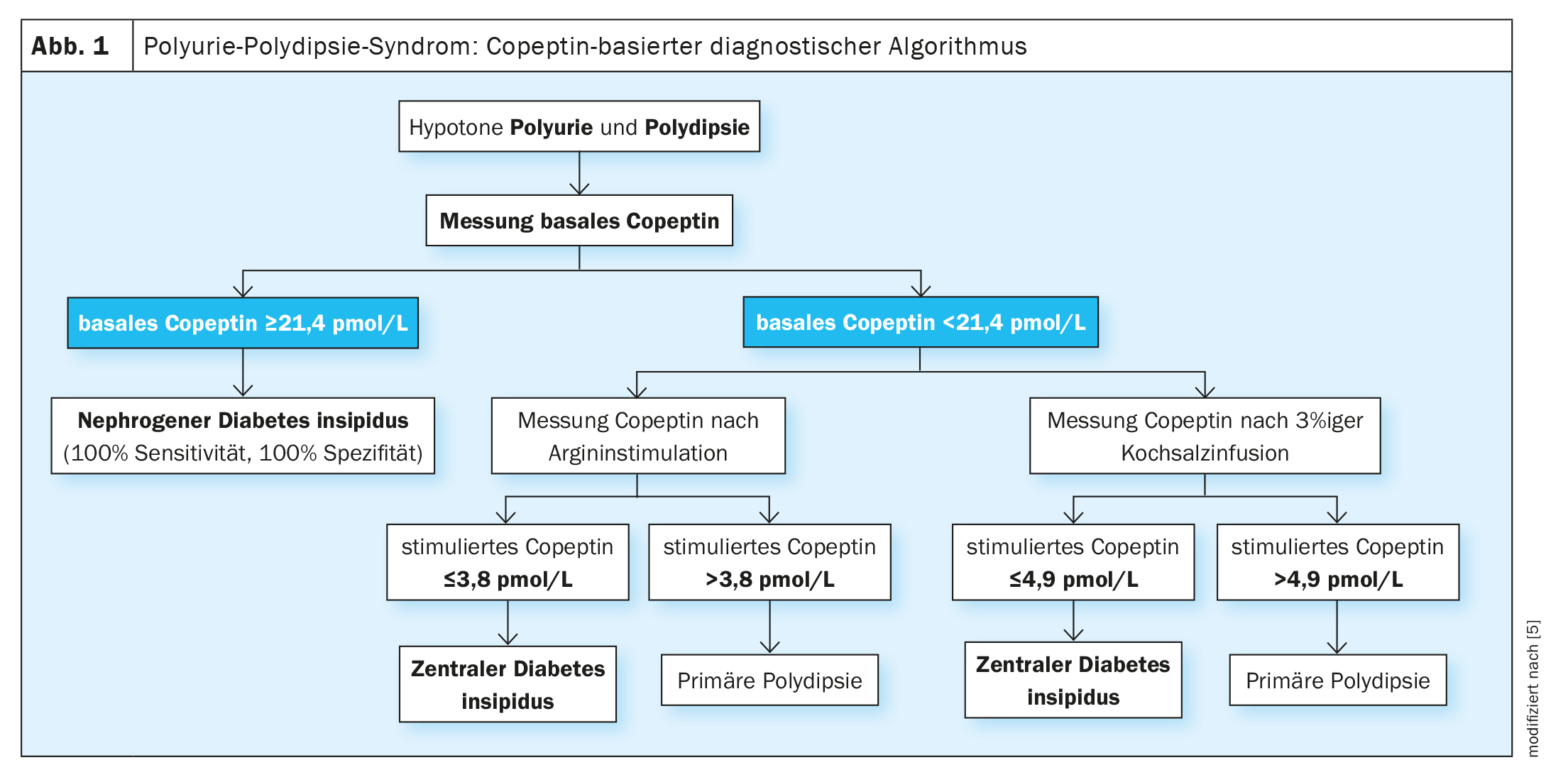
Copeptin as a meaningful surrogate marker of vasopressin.
A copeptin-based algorithm (Fig. 1)is nowadays promoted as the gold standard for the differential diagnosis of polyuria-polydipsia syndrome. Copeptin is a stable and reliable surrogate marker of vasopressin that reflects vasopressin concentration in the circulation. The development of copeptin assays represented a major advance in the differential diagnosis of the polyuria-polydipsia syndrome. Thus, a basal copeptin level without prior thirst can diagnose nephrogenic diabetes insipidus. Osmotic (using hypertonic saline) or nonosmotic (using arginine) stimulation is required to differentiate central diabetes insipidus from primary polydipsia. Both tests allow discrimination between these entities with higher diagnostic reliability than the thirst test. Correct diagnosis is a prerequisite for targeted therapy.
Literature:
- “Drinking by the liter: new test identifies cause of pathologically disturbed fluid balance,” University Medical Center Leipzig, Aug. 02, 2018.
- Chifu I, Fenske W: New Diagnostic Standard in Diabetes Insipidus. Dtsch Med Wochenschr 2018; 143(24): 1739-1744.
- Atila C, et al: Central diabetes insipidus from a patient’s perspective: management, psychological co-morbidities, and renaming of the condition: results from an international web-based survey. Lancet Diabetes Endocrinol 2022; 10(10): 700-709.
- “Diabetes insipidus from the patient’s perspective,” University of Basel, Sept. 15, 2022.
- Christ-Crain M: Copeptin – value in the diagnosis of the polyuria-polydipsia syndrome. J Clin Endocrinol Stoffw 2020; 13: 142-150.
HAUSARZT PRAXIS 2023; 18(1): 32-33