Functional mitral regurgitation (FMR), unlike primary mitral regurgitation, is caused by ventricular dysfunction. Since it is always a consequence of left ventricular disease, optimal drug therapy for heart failure is the first step in the management of these patients. In addition, catheter interventional procedures for therapy have also become established in recent years, including the so-called edge-to-edge repair using the MitraClip system.
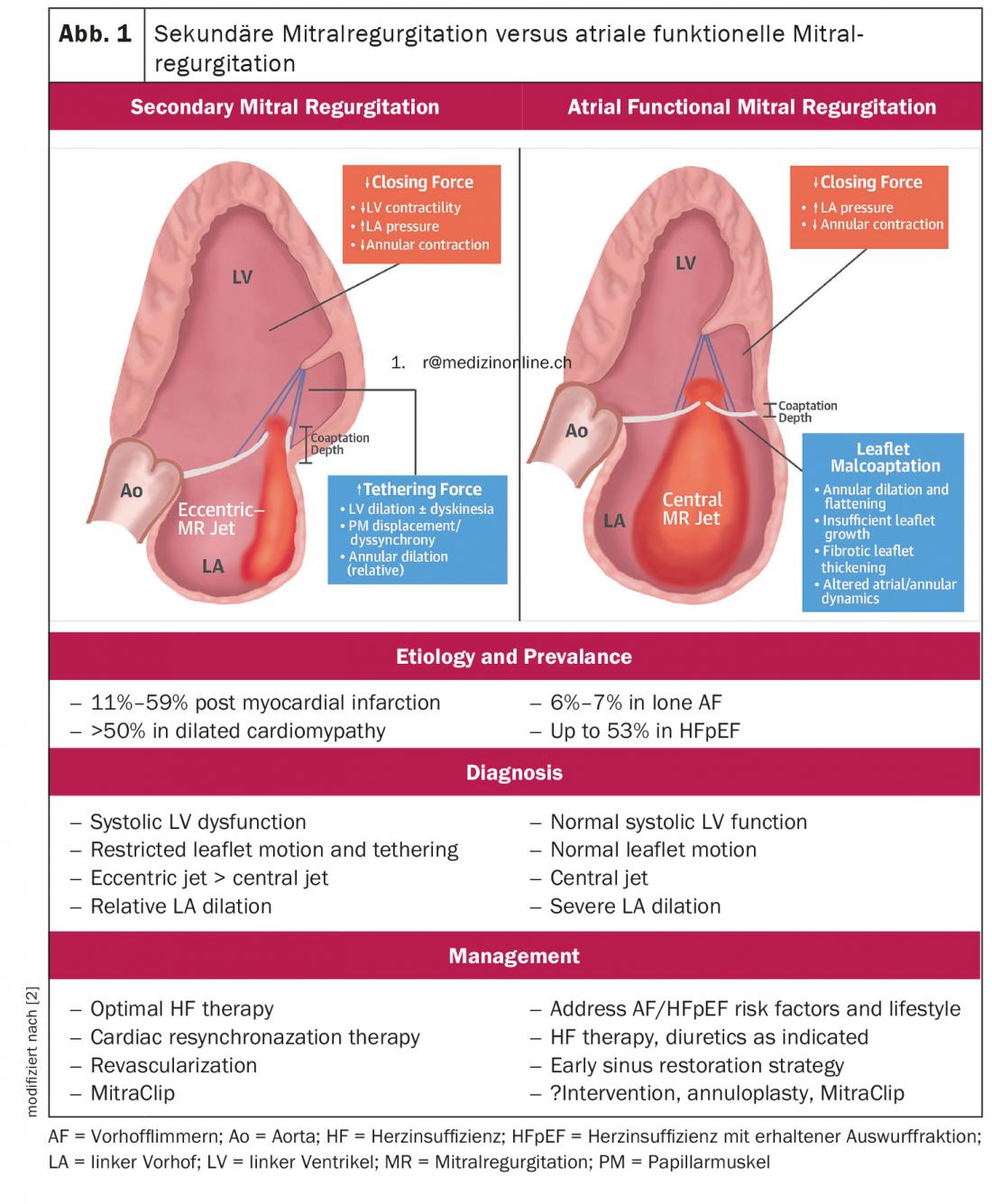
Mitral valve regurgitation represents the second most common adult acquired valvular defect and the most common form of valvular insufficiency. According to their etiology, they are divided into primary (degenerative) and secondary (functional) insufficiencies, with the respective treatment strategy being fundamentally different. In contrast to primary mitral regurgitation, in which the valve per se is affected either by structural abnormalities or degenerative processes of the valve itself, secondary or functional mitral regurgitation (FMR), which occurs in the setting of left ventricular dysfunction, is not only more common and associated with a worse prognosis in patients with heart failure, but the benefit of surgical repair of the valve is also more uncertain compared with primary mitral regurgitation. Previously, FMR was predominantly considered to be based on ventricular disease, either ischemic cardiomyopathy (ICMP) or dilated cardiomyopathy (DCMP). However, in recent years, the diagnosis of functional atrial MI (AFMR) in the setting of left atrial dilatation, usually in the setting of chronic atrial fibrillation, has gained acceptance (Fig. 1) [2]. This is of crucial importance because it allows the pathophysiological classification of the frequently encountered severe MI despite normal ventricular function and geometry as well as normal mobility of the valve leaflets. Furthermore, initial study results suggest that AFMR patients may benefit from therapy.
Therapy option with low periinterventional risk
In light of the existing need for mitral valve therapy in these patients, less invasive interventional therapies that take surgical reconstruction techniques as their model have been established in recent years. The most commonly used method is percutaneous mitral valve reconstruction “edge-to-edge repair” using the MitraClip system (Abbott Vascular), which is a treatment option with low periinterventional risk. In a controlled randomized trial (EVEREST II) that included 279 patients with predominantly primary mitral regurgitation, the MitraClip system was compared with cardiac surgery in a 2:1 randomization. MitraClip therapy was inferior to surgery in terms of reducing insufficiency, but showed superior safety and comparable clinical benefit to surgery even after five years [3]. As for surgical therapy, however, no survival benefit has been shown for the MitraClip procedure in controlled trials compared with drug therapy alone. To date, only a post hoc analysis from the EVEREST II study and a monocentric, retrospective, propensity-matched study suggesting equivalence to surgical therapy and superiority to drug therapy existed in this regard.
Revealing the controversy between COAPT and MITRA-FR.
The results of two recent randomized controlled trials (COAPT and MITRA-FR) comparing conservative and MitraClip therapy have been contrasting. In the COAPT trial, percutaneous mitral valve repair with the MitraClip reduced all-cause mortality and hospitalization in patients with at least moderate to severe mitral regurgitation compared with guideline-recommended medical therapy alone. However, data from the concurrently published MITRA-FR trial showed no prognostic benefit for patients with advanced heart failure and severely enlarged left ventricle, so MitraClip treatment should be performed only after careful patient selection and decision-making by the heart team [4,5].
Patient selection criteria
According to Prof. Dr. Dr. Philipp Lurz, Managing Senior Physician in the Department of Cardiology at the Heart Center Leipzig, the selection of a patient with FMR for transcatheter treatment therefore depends on various aspects. These include, first, the severity of mitral regurgitation and left ventricular dysfunction, and the optimization of guideline-directed medical therapy (GDMT) [1]. Thus, optimal drug therapy for heart failure and, if indicated, implantation of a resynchronization pacemaker (CRT system) are still the cornerstones of therapy for functional mitral regurgitation. However, even with optimal drug and CRT therapy, a majority of patients remain with symptomatic severe mitral regurgitation. According to the guideline, when revascularization is not indicated and the surgical risk is not low, a percutaneous edge-to-edge procedure can be performed in patients with severe secondary mitral regurgitation and an LVEF >30% who remain symptomatic despite optimal medical management (including CRT if indicated) and in whom echocardiography shows appropriate valve morphology to avoid futility should be considered. Transcatheter edge-to-edge repair (TEER) should be considered in selected symptomatic patients who are not candidates for surgery and meet criteria suggesting an increased chance of response to therapy [6].
Take-Home Messages
- Functional mitral valve regurgitation is associated with heart failure.
- Drug therapy is always the first choice of treatment.
- Interventional therapy options are a good option in case of non-response to drug therapy.
Congress: DGIM Interdisciplinary Clinical Symposium
Literature:
- Prof. Dr. Dr. Philipp Lurz: Interventional mitral valve therapy – where do we stand today and what about residual tricuspid regurgitation, DGIM Interdisciplinary Clinical Symposium, 04/30/2022.
- Dferm S, et al: Atrial Functional Mitral Regurgitation: JACC Review Topic of the Week. JACC 2019; https://doi.org/10.1016/j.jacc.2019.02.061.
- Mauri L, et al: The EVEREST II Trial: design and rationale for a randomized study of the evalve mitraclip system compared with mitral valve surgery for mitral regurgitation. Am Heart J 2010; doi: 10.1016/j.ahj.2010.04.009.
- Stone GW, et al: Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 2018; doi: 10.1056/NEJMoa1805374.
- Obadia JF, et al: Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N Engl J Med 2018; doi: 10.1056/NEJMoa1805374.
- Vahanian A, et al: 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal 2022; doi: https://doi.org/10.1093/eurheartj/ehac051.
CARDIOVASC 2022; 21(3): 24-25