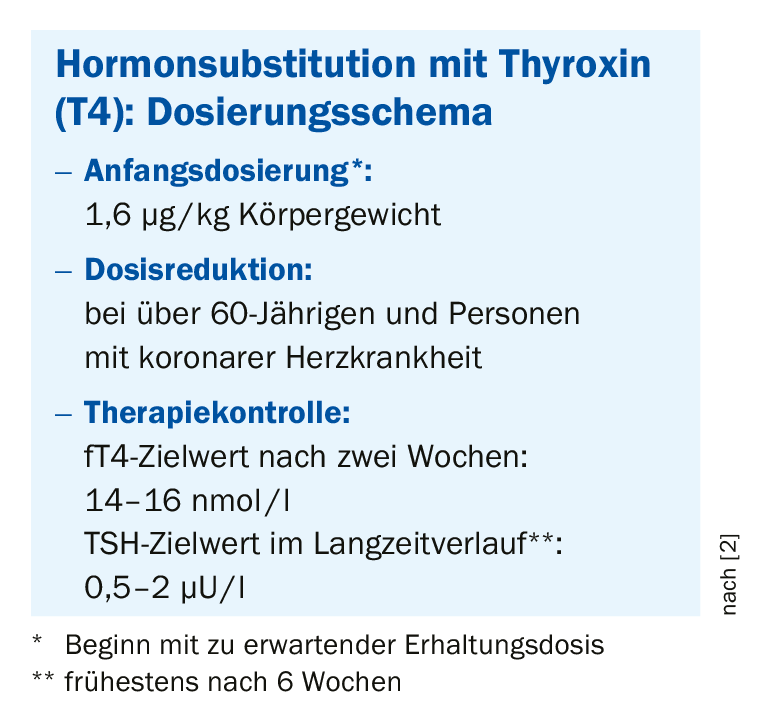
Hormone replacement therapy is still considered the standard treatment for hypothyroidism. Attention should be paid to an adequate dosage regimen. Dose reduction is indicated in those over 60 years of age and in patients with coronary artery disease.
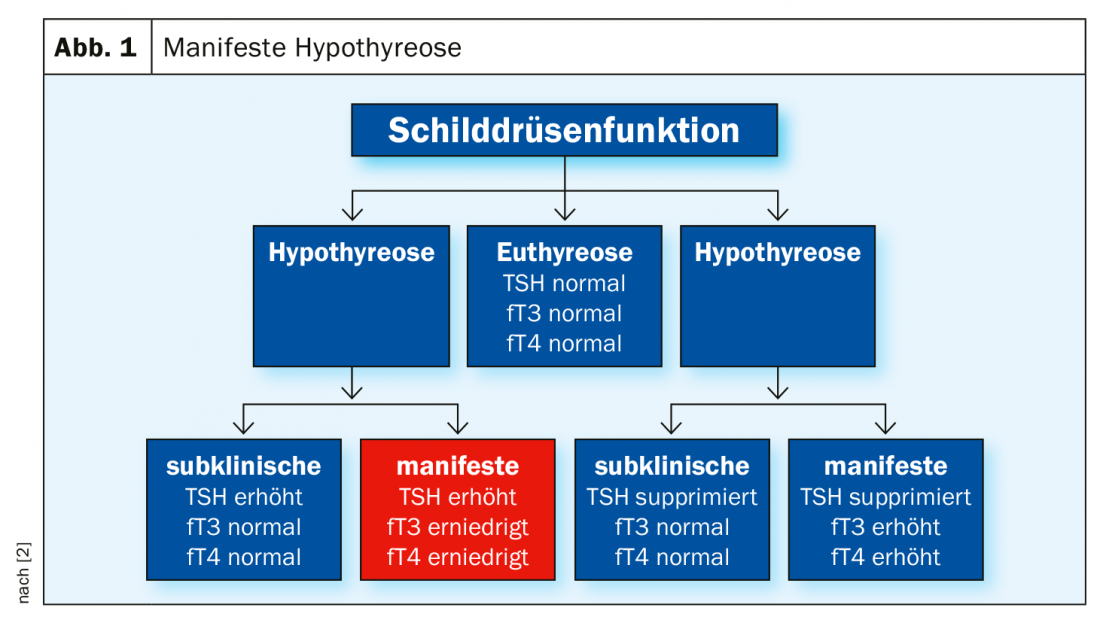
Hypothyroidism is more common than hyperthyroidism, in Europe the prevalence in the general population is about 4% resp. 1% for hyperthyroidism [1,2]. In hypothyroidism, TSH levels are too high and free thyroxine (fT3 and fT4) too low (Fig. 1). Typical symptoms of manifest hypothyroidism include fatigue, listlessness and hypothermia. Other clinical signs include arterial hypertension (especially elevation of diastolic BP) and hyporeflexia, as well as changes in voice (deep, hoarse) and skin (pale). “In old age, hypothyroidism is often oligosymptomatic,” explains Prof. Roger Lehmann, MD, Senior Physician at the Department of Endocrinology, Diabetology and Clinical Nutrition at the University Hospital Zurich [2]. In very rare cases, hypothyroid coma may develop (loss of consciousness, bradypnea). If only the TSH value is elevated, but the peripheral values are normal, this is called subclinical hypothyroidism. Since sufficient thyroid hormones are still produced, there are usually no associated symptoms, but the risk of progression to manifest hypothyroidism is increased. TSH values <5 mU/l are considered the normal range; a clear indication for substitution therapy (Eltroxin®, Euthyrox®) are TSH values >10 mU/l.(Box). The following dosing regimen has proven effective: Start with the expected maintenance dose respectively 1.6 µg/kg body weight, 30 minutes before breakfast [2]. The latter is important because otherwise the drug can be metabolized much less well, the speaker explains. Dose reduction should be made in those over 60 years of age and those with coronary artery disease. If the target values are reached after two weeks, the control interval can be extended. If necessary, a dose adjustment must be made during the course.
Hashimoto’s syndrome is a common cause
In about 40% of cases, hypothyroidism is due to autoimmune thyroiditis. This is a chronic inflammatory disease of the thyroid gland, which is called Hashimoto’s syndrome or chronic lymphocytic thyroiditis. Initially, hyperthyroidism occurs (hashitoxicosis), and later, hypothyroidism develops. In the hypertrophic form of Hashimotos syndrome, diagnostic markers include lymphocytic infiltrates and antibodies to a thyroid enzyme (TPO positive in 80-99%, TAK positive in 35-60%) and diffuse goiter. The second most common cause is idiopathic with more than one third. The third most frequent cause is post-therapeutic hypothyroidism, e.g. after radiation or after total/subtotal thyroidectomy. Among the substances that can trigger drug-induced hypothyroidism is amiodarone. However, the arrhythmic drug does not have to be discontinued; the hypothyroidism can be corrected by substitution therapy with Eltroxin® or Euthyrox®. Thyrostatic drugs, lithium, interferon-α, interleukin-2, and tyrosine kinase inhibitors (checkpoint inhibitors: sunitinib, sorafenib) are other agents that can lead to hypothyroidism. Only rarely occurring in Switzerland are congenital hypothyroidism (cretinism).
Euthyroid Sick Syndrome often occurs in states of weakness
A drop in thyroid hormones is a characteristic allostatic constellation of the thyrotropic control circuit that often occurs in states of starvation and in severe acute or chronic illness. This is called euthyroid sick syndrome or non-thyroidal illness syndrome. This is almost always seen in patients in the ICU, the speaker said. TSH and fT3 (half-life of one day) decrease more rapidly than fT4, which has a half-life of one week. In the convalescent phase, thyroid hormone production is stimulated and there is an increase in TSH (up to 20 mU/l) [3]. Therefore, thyroid levels should be measured repeatedly during this phase. For example, a month later, a previously excessive TSH level may be back within the normal range. In terms of iodine requirements, an adult needs about 150 µg of iodine per day, which in Switzerland is normally covered by the consumption of iodine-containing salt [2].
Literature:
- Madariaga AG, et al: The Incidence and Prevalence of Thyroid Dysfunction in Europe: A Meta-Analysis. J Clin Endocrinol Metab 2014; 99: 923-931.
- Lehman R: Hypo- and Hyperthyroidism, Prof. Dr. med. R. Lehmann, FOMF Internal Medicine, Zurich, 24.06.2020.
- Lehmann R: Hypo- and Hyperthyroidism, Prof. Dr. med. R. Lehmann, FOMF Internal Medicine, Zurich 04.12.2019.
GP PRACTICE 2020; 15(7): 50