In addition to the groundbreaking new discovery of dapagliflozin as an effective and safe add-on therapy option in heart failure, there are several other interesting updates. Potassium levels are an important parameter in aldosterone antagonist therapy. Regarding creatinine, the current consensus is that an increase of 30-50% is tolerable. Left bundle branch block and QRS complex are important criteria for the indication of cardiac resynchronization therapy.
Heart failure is mainly treated with medication with the aim of slowing down the progression of the disease, taking the strain off the heart and improving the patient’s quality of life. The old truism that optimal up-titrating is an important therapeutic principle in the treatment of heart failure patients is still valid today, explains Prof. Otmar Pfister, MD, Cardiology Clinic, University Hospital Basel [1]. As a result, a mortality reduction of up to 30% can be achieved. Therefore, it is important to see patients on a regular basis.
Dapagliflozin as a new add-on therapy
The latest finding in the field of drug therapy options for heart failure is that the SGLT-2 inhibitor dapagliflozin, developed for diabetes therapy, has a beneficial effect. The DAPA-HF trial (“Dapagliflozin And Prevention of Adverse-outcomes in Heart Failure trial”) showed that dapagliflozin in combination with standard therapy significantly reduced the risk of mortality and hospitalization [2]. This was a prospective randomized, placebo-controlled trial in patients with heart failure and reduced ejection fraction (HFrEF) whose left ventricular ejection fraction (LVEF) was ≤40%. Study participants were randomly assigned to dapagliflozin 10 mg daily (n=2373) or placebo (n=2371) as an adjunct to standard therapy, regardless of diabetes status [2]. The speaker pointed out that overall the subject collective received very good standard therapy. The follow-up period was 18.2 months. In the dapagliflozin add-on condition, a significant relative risk reduction (RRR) of 26% in cardiovascular death or hospitalization due to myocardial infarction was achieved, with a “number needed to treat” of only just 21, as the speaker pointed out [2]. No serious adverse events occurred and tolerability did not differ significantly according to age (mean age: 66 years) [2]. For standard therapy, ACE inhibitors, angiotensin receptor blockers (ARBs), renin antagonists, angiotensin receptor neprilysin inhibitors (ARNIs), and beta blockers continue to play an important role. In severe heart failure and persistent respiratory distress, aldosterone receptor antagonists may be prescribed under certain conditions. This mildly diuretic substance has a positive effect on long-term prognosis. ARNIs may be used when therapeutic goals are not achieved with angiotensin receptor antagonists.
Monitoring of potassium levels is important
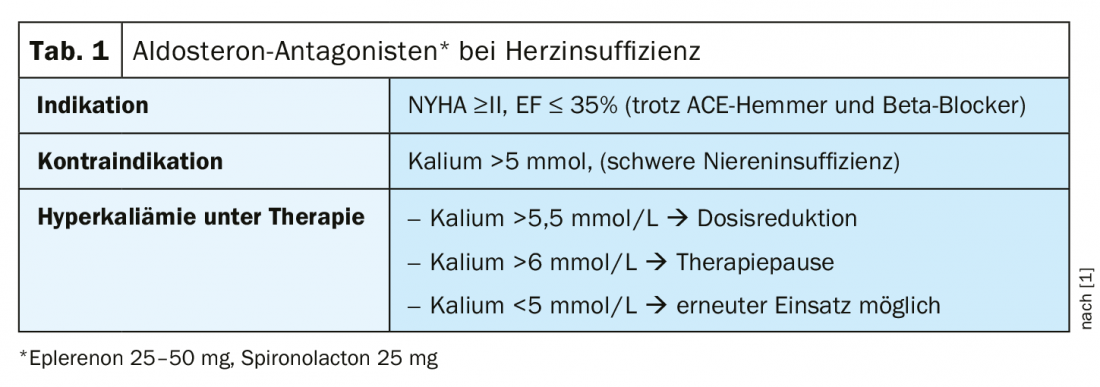
If the potassium value is above 5 mmol/L, this is a contraindication for aldosterone antagonists. If the potassium increases during the course of therapy, the speaker recommends following the rule below: At a potassium value >5,5 mmol/L halve the dose if >6 mmol/L pause therapy and do not restart until a value of <5 mmol/L is reached (tab. 1) . The following applies to diuretics: as much as necessary, but as little as possible. Prof. Pfister advises, especially in elderly patients, to take blood pressure measurements while sitting and standing in order to detect any orthostasis and to reduce diuretics if necessary. With regard to ACE inhibitors/ARNI/betablockers, the motto is “start low, go slow, aim high” – one should successively increase an initial low dosage and start beta-blockers only after recompensation in an evolemic state. One question he frequently encounters in clinical practice is whether or not to discontinue ACE inhibitors/ARNIs when creatinine rises. The answer to this is that there is no need to stop therapy immediately, but a creatinine increase of 30-50% is tolerable, explains the speaker [1], at most the dose can be halved.
Whether and when in the course of therapy to switch from ACE inhibitors to sacubitril/valsartan should be investigated in the PIONEER-HF trial [3], The data suggest that sacubitril/valsartan should be used as early as possible in the postacute decompensation phase to optimize the management of chronic heart failure in the clinic and reduce the likelihood of re-hospitalization or cardiovascular events. According to current data, the best effect can be achieved with sacubitril/valsartan in patients with systolic heart failure HFrEF. Thus, a significant improvement in prognosis was demonstrated in this patient group compared with ACE inhibitors in the PARADIGM-HF trial [4]. These findings were replicated in a U.S. study published in 2020. Compared with ACE/ARB, sacubitril/valsartan was associated with a lower risk of mortality and hospitalization in this heterogeneous patient cohort [5].
Cardiac resynchronization therapy or defibrillator indicated?
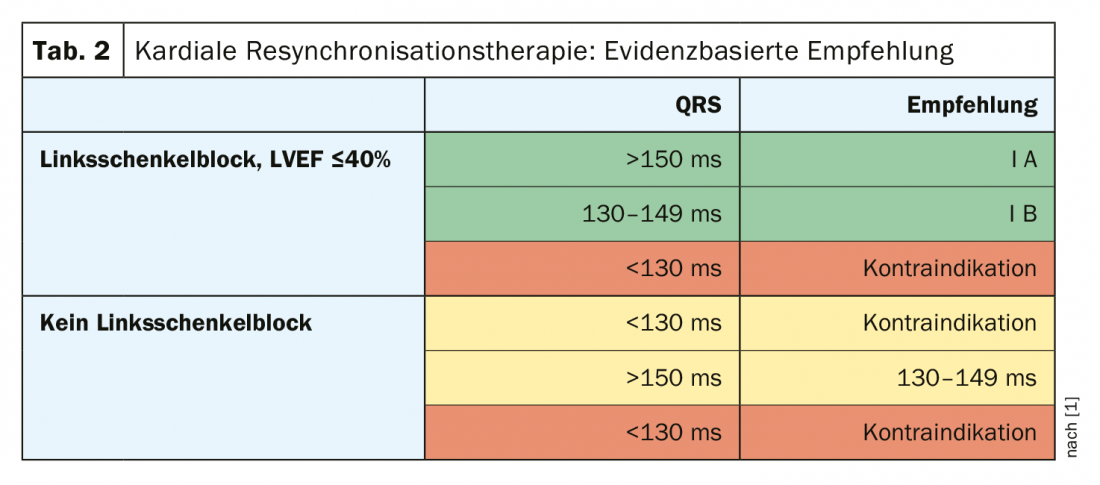
In cases of advanced heart failure and additional conduction delay of the electrical activation of the heart (evident by a widened QRS complex in the ECG), biventricular pacing, which resynchronizes the work of the ventricles and thus increases the pumping capacity of the heart without a simultaneous increase in oxygen consumption, may be useful. This has been shown to reduce re-hospitalizations and mortality and increase quality of life [7]. However, the rate of non-responders is approximately 25-30%, and patients should be informed of this [1]. A class IA indication exists for left bundle branch block (LVEF ≤40%) and QRS >150 ms; these patients may benefit greatly. A Class IB recommendation is present at QRS 130-149 ms (Table 2) [1,6]. At an LVEF ≤35%, there is an indication for a defibrillator in symptomatic patients. “But you have to look at it individually,” the speaker explains. A defibrillator (ICD) is particularly suitable for people with ischemic heart disease, as they have a significantly increased risk of sudden cardiac death. In contrast, the risk is less in patients with nonischemic cardiopathy, and there is evidence that the benefit of ICD in this patient group is significantly less in those >65 years of age.
Source: FOMF Basel
Literature:
- Pfister O: Guideline-based therapy of heart failure. Prof. Otmar Pfister, MD, University Hospital Basel, FOMF Basel, Jan. 31, 2020.
- Mc Murray JJV, et al: Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med 2019; 381: 1995-2008.
- Morrow DA, et al: Clinical Outcomes in Patients With Acute Decompensated Heart Failure Randomly Assigned to Sacubitril /Valsartan or Enalapril in the PIONEER-HF Trial. Circulation 2019; 139(19): 2285-2288.
- McMurray JJ, et al: Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 2014; 371(11): 993-1004.
- Tan NY, et al: Comparative Effectiveness of Sacubitril-Valsartan Versus ACE/ARB Therapy in Heart Failure With Reduced Ejection Fraction. Heart Fail 2020; 8(1): 43-54.
- ESC (European Society of Cardiology): Clinical Practice Guidelines, www.escardio.org/Guidelines/Clinical-Practice-Guidelines, last accessed 6/10/2020.
- Goldenberg I, et al: Survival with Cardiac-Resynchronization Therapy in Mild Heart Failure. N Engl J Med 2014; 370: 1694-1701.
HAUSARZT PRAXIS 2020; 15(7): 52-53 (published 7/28/20, ahead of print).











