When talking about headaches, not necessarily always the same pain is meant. It is much more likely that symptoms present differently from patient to patient. More than 200 different types of headache are now defined. What they have in common is the significant reduction in the quality of life of those affected. Therapy should therefore be comprehensive and adapted to the headache in question.
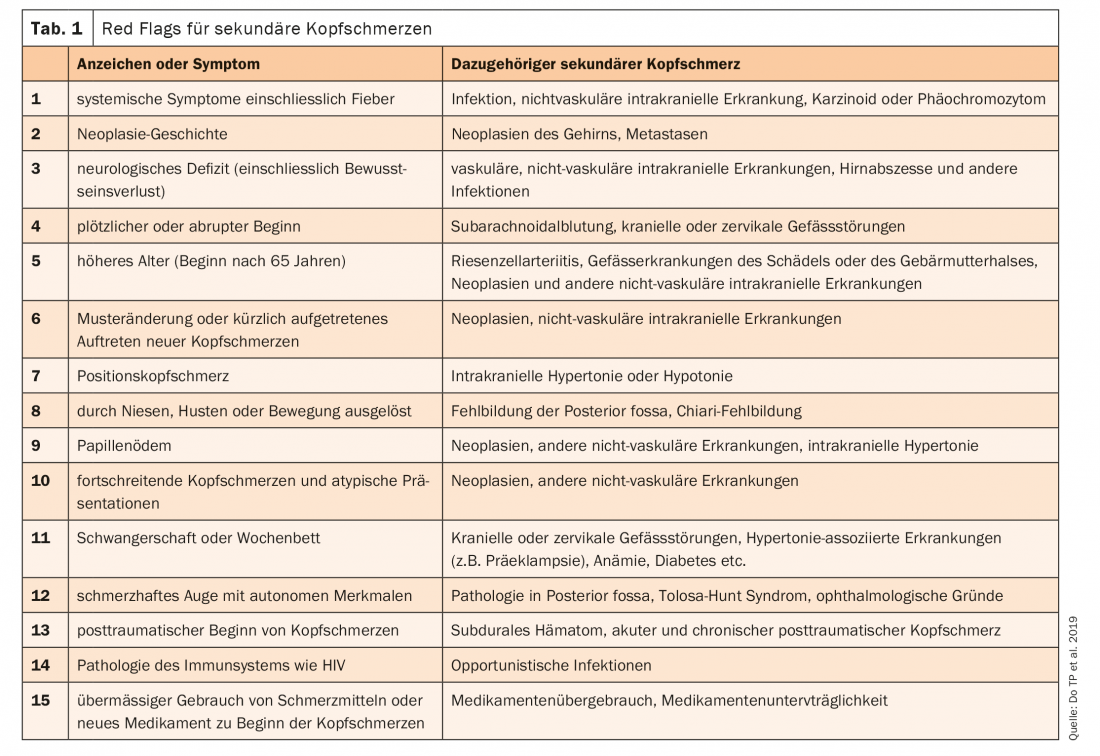
The International Classification of Headache Disorders (ICHD-3) divides headache into primary and secondary headaches, as well as neuropathies and facial pain [1]. In total, more than 200 different types of headache are recorded, which have been grouped into 14 groups. By far the most widespread are tension headaches, followed by migraine, as PD Dr. med. Andreas R. Gantenbein, Bad Zurzach, pointed out. Indeed, only a minority of an estimated 18% worldwide suffer from secondary headaches [2]. Therefore, they are often overlooked. Red flags can be used to increase the likelihood of identifying a secondary etiology (Table 1) [2]. This includes checking for systemic symptoms such as fever, neurologic deficits, or sudden onset, among others. If secondary triggers for the complaints can be excluded, the primary headache must be declared accordingly.
Cluster headaches occur unilaterally around the eye over a four-hour period. The pain peak is reached after about three hours. Eye redness, tearing as well as a blocked nose are noticeable. “Sufferers also frequently “putter” around during the attack,” the expert said. Acute therapy can be given via triptans as a nasal spray as well as O2 administration. To prevent cluster headaches, administration of verapamil, topiramate, lithium, galcanezumab, or prednisone is possible.
Treat migraine effectively and comprehensively
Migraine can be clearly distinguished from tension headaches. Tension headaches are dull, diffuse bilaterally, and mild to moderate in intensity, with no accompanying symptoms. Migraine, on the other hand, is usually unilateral, pulsatile, and is often accompanied by nausea/vomiting and photo/phonophobia. The pain occurs over four to 72 hours and intensifies with movement. Trigger factors, such as the weather, cheese or red wine, among others, can trigger an attack. “During a migraine, rest, sleep and relaxation are most important,” Gantenbein reported. Medication can be used to treat an acute attack with analgesics, NSAIDs, antiemetics, or triptans. The important thing here is that the dose is targeted and high enough, but not taken too frequently. First-line agents for patients with moderate to severe attacks are triptans [3]. However, these may be contraindicated in some patients. Especially in patients with a history of stroke or myocardial infarction. In addition, patients with severe hypertension, coronary artery disease, peripheral arterial occlusive disease (CAD) or transient ischemic attack (TIA) must also avoid this substance class. This is because triptans do not contract intracranial blood vessels exclusively, but also peripheral blood vessels. Two new substance classes are waiting in the wings: Ditane and Gepante. Although the former also target the serotonin receptor, they act selectively at 5-HT1F. Gepante are small molecules that act as antagonists at the CGRP receptor.
Prophylaxis for frequent seizures
If patients suffer from migraines several times a month with very severe or prolonged attacks, prophylactic treatment should be considered. Also, to prevent medication overuse, which in turn can end in headaches. In addition to aerobic endurance training, relaxation therapies and behavioral and psychotherapeutic measures, drug interventions may be effective. Attention should be paid to comorbidities. Beta-blockers are contraindicated in patients with severe asthma or hypotension, for example. In addition, beta-blockers, flunarizine, and topiramate can promote depression. On the other hand, the blood pressure- and pulse-lowering effect of beta-blockers can also be a desirable side effect. Topiramate may promote weight loss, and amitriptyline has a sedative effect. In principle, antidepressants, anticonvulsants, beta-blockers, calcium antagonists, and CGRP antibodies can be used for migraine prophylaxis. Natural substances such as magnesium, coenzyme Q10 and riboflavin or the administration of botulinum toxin type A can also contribute to preventive therapy [3].
Congress: Forum for Continuing Medical Education
Literature:
- www.ichd-3.org (last accessed on 13.02.2021)
- Do TP et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology 2019; 92(3): 134-144.
- Therapy recommendations of the Swiss Headache Society. Available at: www.headache.ch/download/Content_attachments/FileBaseDoc/SKG_Therapieempfehlungen_2018_DE_15_WEB.pdf (last accessed on 13.02.2021)
InFo NEUROLOGY & PSYCHIATRY 2021; 19(2): 22-23 (published 3/30/21, ahead of print).