Iron deficiency is a common comorbidity in patients with heart failure and is associated with increased mortality and hospitalizations. Effective iron supplementation significantly reduces this risk without increasing the risk of adverse events.
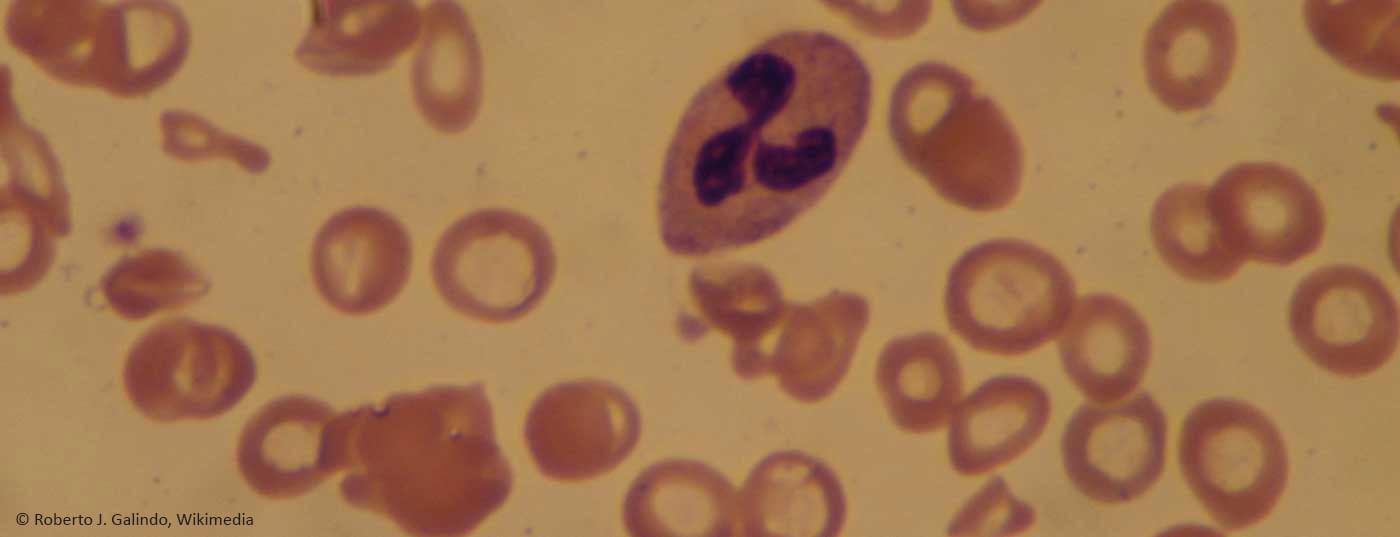
Iron deficiency is the most common deficiency disease in humans. About 600 million people worldwide suffer from iron deficiency of various causes. Iron deficiency is also a common and relevant comorbidity in chronic heart failure. It affects symptoms, quality of life, and hospitalization rates and is a negative prognostic factor. Clinical symptoms of iron deficiency include fatigue, lassitude, performance insufficiency, shortness of breath, cognitive dysfunction, dizziness, headache, and susceptibility to infection, as well as a general impairment of quality of life. Approximately 50% of patients with chronic heart failure suffer the consequences of iron deficiency. Via peripheral vasodilation, blood pressure drop and activation of neurohormones, chronic anemia can trigger a veritable vicious circle.
Several mechanisms are discussed regarding the causes of iron deficiency in heart failure, including chronic inflammation, decreased iron absorption, decreased reabsorption of iron, and last but not least, drug-induced bleeding anemia. In addition, NYHA stage appears to correlate with iron deficiency. Absolute iron deficiency is defined as serum ferritin <100 μg/l, functional iron deficiency is present with serum ferritin 100-300 μg/l with concomitant transferrin saturation <20%.
Iron deficiency mainly affects the patient’s quality of life through symptom worsening of heart failure, physical performance, muscle function, and the number of hospitalizations due to worsening heart failure. This is because iron is necessary for optimal hematopoiesis, but also plays a central role in oxygen transport (hemoglobin), storage (myoglobin), metabolism of cardiac and skeletal muscles, synthesis and degradation of proteins, lipids, ribonucleic acids, and mitochondrial function.
Balance quickly, effectively and safely
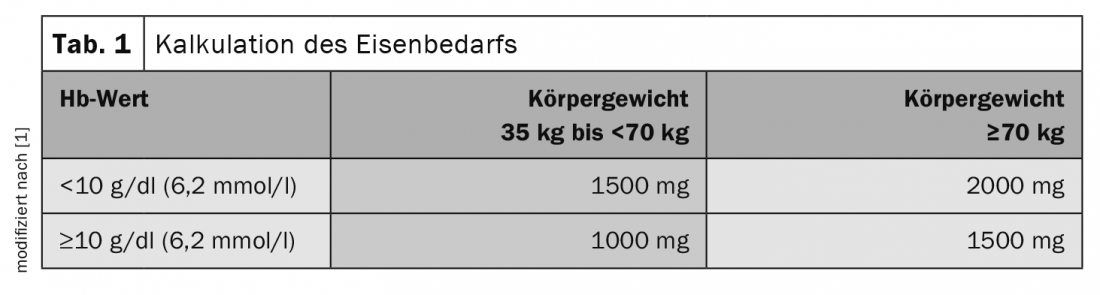
Iron requirements in patients with chronic heart failure can be determined as a function of body weight and hemoglobin level (Tab. 1). Oral iron substitution, which is normally considered the drug of choice, is poorly absorbed, especially in patients with chronic diseases such as heart failure, and have limited bioavailability. In addition, tolerability is limited due to unfavorable gastrointestinal effects. Several months of oral iron therapy would be required to replicate the iron deficiency.
Therefore, intravenous iron therapy should be resorted to. Compared to the old preparations, the dextran-free complexes now available show anaphylactic reactions extremely rarely and can be infused relatively quickly due to their high structural stability – both properties that also allow their use in the outpatient setting.
Literature:
- Link H, Schiefke I, Balck K, et al: Diagnostic and treatment principles of iron deficiency anemia. MMW Fortschr Med 2015; 157: 56-59.
CARDIOVASC 2021; 20(4): 31