At the annual meeting of the Swiss Society of Pneumology (SGP) in Interlaken, one of the topics was COPD. Exacerbations in particular were the subject of discussion. How exactly are they defined and what are the associated factors? Is five days of systemic glucocorticoid therapy already effective in reducing the risk of further exacerbations? In addition, the current therapeutic landscape of COPD in general was discussed.
(ag) Several events were dedicated to exacerbations in chronic obstructive pulmonary disease (COPD). Peter Grendelmeier, MD, from the University Hospital of Basel, Switzerland, first discussed the definition of an exacerbation: According to the 2014 GOLD report, an exacerbation is an acute event characterized by worsening respiratory symptoms. This worsening exceeds the normal symptom variations of the disease and it leads to a change in medication.
For example, in moderate severity, treatment with systemic corticosteroids, antibiotics, or both is reasonable; in severe cases, hospitalization becomes necessary. Consequences of exacerbations, according to Dr. Grendelmeier, include negative affect on quality of life, several weeks of recovery time, association with increased mortality [1], long-term lung function decline [2], and high socioeconomic costs.
Possible factors associated with exacerbation in COPD were also presented at the annual meeting. A cohort study by Nebal Abu-Hussein et al., Kantonsspital Baselland/Liestal, concluded that especially previous exacerbations and current severe symptoms such as sputum production, severe dyspnea and chronic cough are important predictors for future exacerbations.

Is as little as five days of prednisone enough?
Prof. Dr. med. Jörg Daniel Leuppi from the Cantonal Hospital Baselland/Liestal presented the randomized, placebo-controlled REDUCE trial [3] published last year, which investigated whether five-day systemic glucocorticoid therapy is equally good and efficient as 14-day systemic glucocorticoid therapy (“non-inferiority”) in the context of exacerbations. Specifically, the question was whether a shorter treatment duration (group 1: 5 days 40 mg prednisone/tgl. plus 9 days of placebo/tgl.) produces the same good results as 14 days of therapy (group 2: 14 days 40 mg prednisone/tgl.) in terms of recurrence of exacerbation in the following six months.
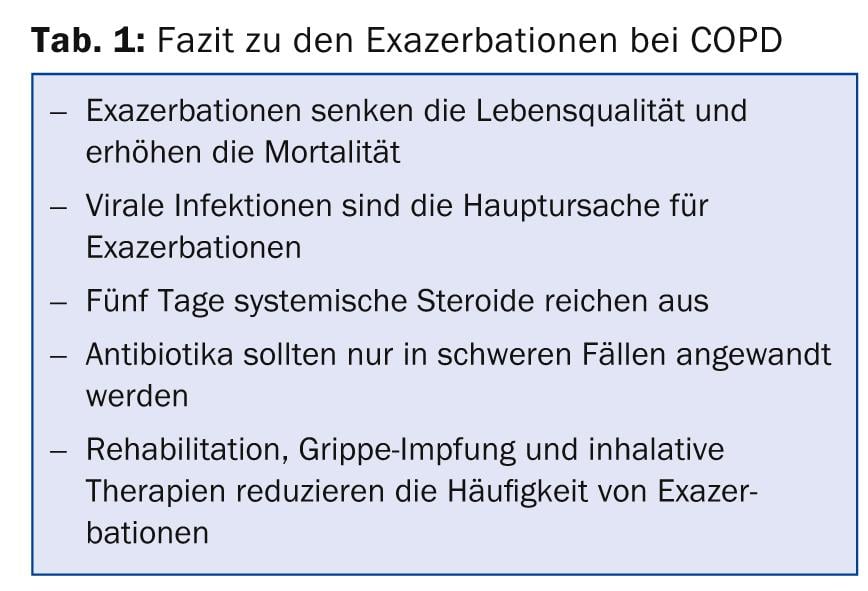
Results: According to Prof. Leuppi, about one-third of patients in each of the two treatment arms suffered a new COPD exacerbation during the six-month observation period (primary endpoint): The exact number was 35.9 in the first group and 36.8% in the second. Consequently, there was no difference whether the COPD exacerbation was treated with 40 mg prednisone/tgl for 5 or for 14 days. has been treated. Similarly, there was no difference in mortality or improvement in pulmonary function. Re-exacerbation occurred at a median of 43.5 days in group 1 and 29 days in group 2. “Our study clearly shows that five-day glucocorticosteroid therapy is not inferior to longer-duration glucocorticosteroid therapy in the treatment of COPD exacerbation. This in a patient population with a majority of severe to very severe COPD,” Prof. Leuppi concluded (Table 1).
Developments of the inhalatives
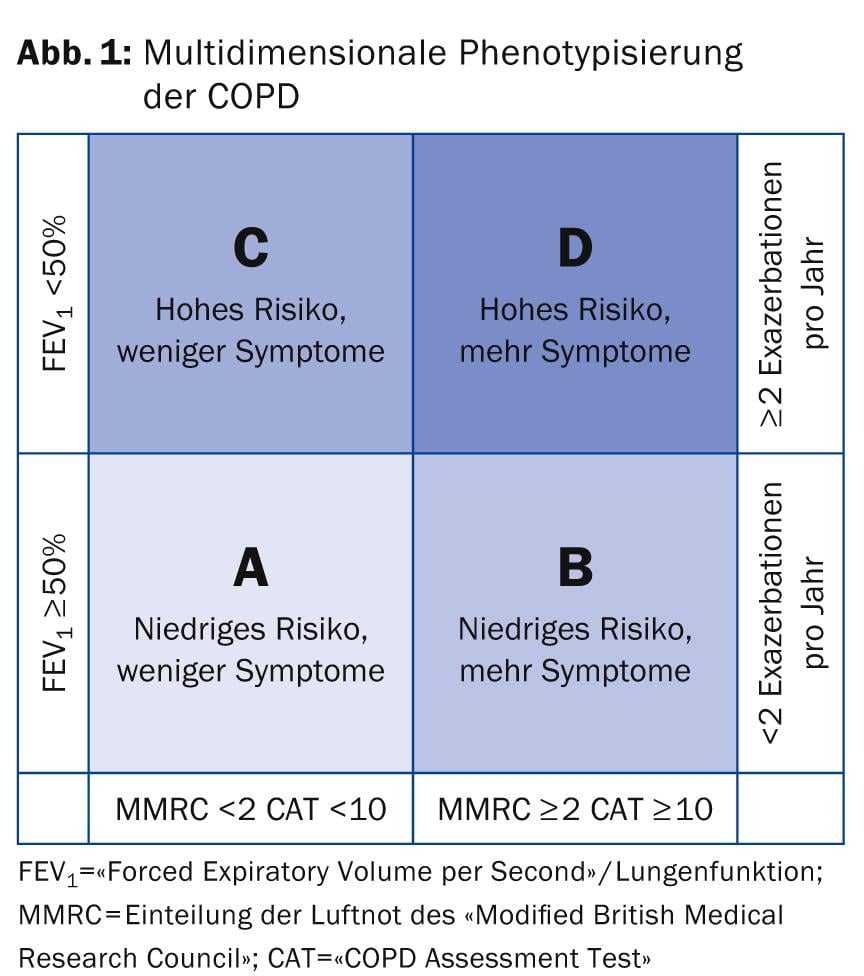
The new multidimensional phenotyping of COPD is shown in Figure 1. Depending on the severity, different first-line therapies are recommended:
- A: short-acting anticholinergic if needed or short-acting β-2-agonist if needed.
- B: long-acting anticholinergic (LAMA) or long-acting β-2-agonist (LABA).
- C: inhaled corticosteroid (ICS) + long-acting anticholinergic (LAMA) or long-acting β-2-agonist (LABA).
- D: inhaled corticosteroid (ICS) + long-acting anticholinergic (LAMA) and/or long-acting β-2-agonist (LABA).
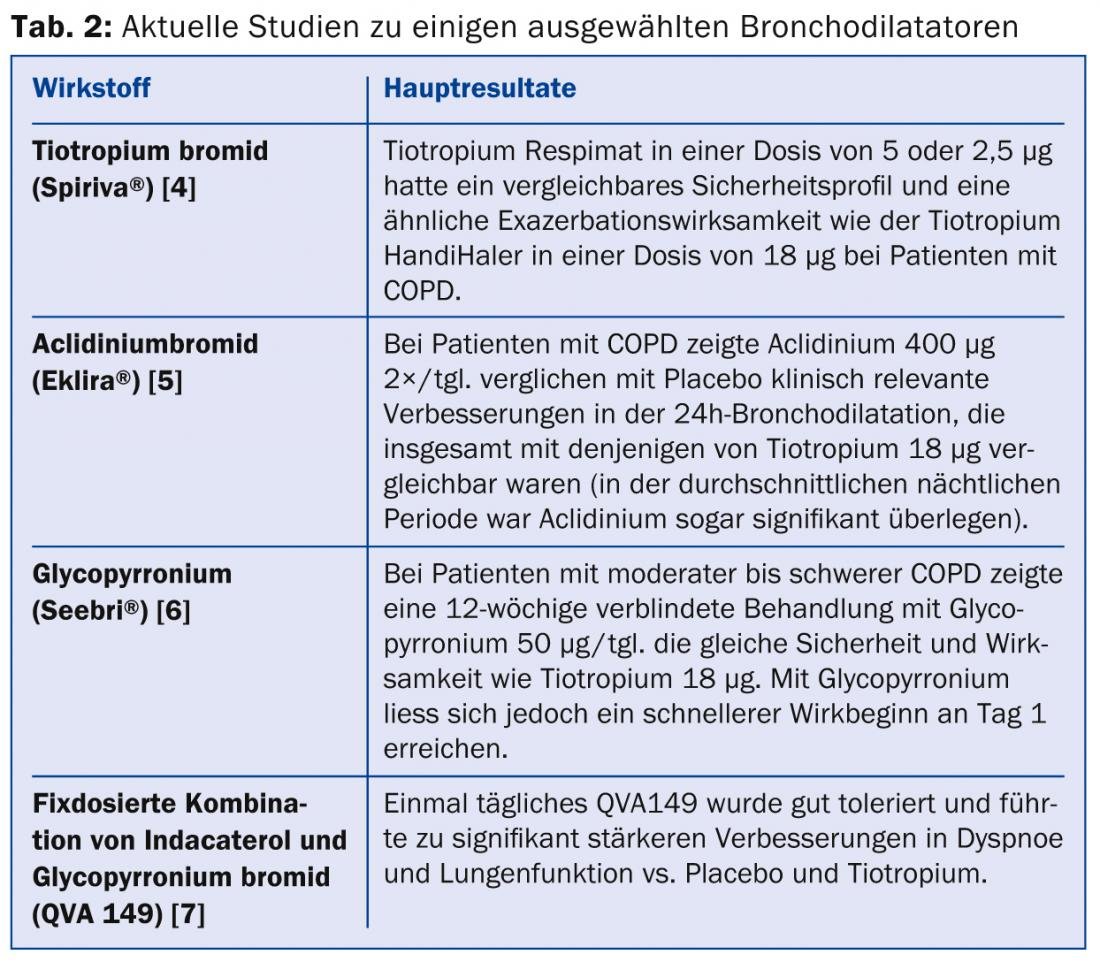
According to Prof. Erich W. Russi, MD, Zurich, the benefits of current inhaled pharmacotherapy include improved lung function, exercise tolerance, and quality of life, as well as a reduction in the frequency of exacerbations in COPD. The new drugs and inhalation devices currently coming onto the market bring rather small benefits, but are nevertheless highly welcome as they expand the therapeutic toolbox. For individual patients, a preference for a drug within the spectrum arises primarily from emotional impressions rather than verifiable differences. “So bronchodilators continue to be the cornerstone of COPD therapy, and dual bronchodilators are even more effective,” Prof. Russi concluded. Some recent studies on the different bronchodilators are mentioned in Table 2. Inhaled corticosteroids (ICS) are used too frequently, according to the expert.
Source: Joint Annual Meeting of the Swiss Society of Pneumology (SGP), the Swiss Society of Pediatric Pneumology (SGPP), the Swiss Society of Thoracic Surgery (SGT) and the Swiss Association of Endoscopy Personnel (SVEP), May 8-9, 2014, Interlaken.
Literature:
- Soler-Cataluña JJ, et al: Thorax 2005 Nov; 60(11): 925-931. epub 2005 Jul 29.
- Donaldson GC, et al: Thorax 2002 Oct; 57(10): 847-852.
- Leuppi JD, et al: JAMA 2013 Jun 5; 309(21): 2223-2231.
- Wise RA, et al: N Engl J Med 2013 Oct 17; 369(16): 1491-1501.
- Fuhr R, et al: Chest 2012 Mar; 141(3): 745-752.
- Chapman KR, et al: BMC Pulm Med 2014 Jan 17; 14: 4. doi: 10.1186/1471-2466-14-4.
- Mahler DA, et al: Eur Respir J 2013 Oct 31 [Epub ahead of print].
HAUSARZT PRAXIS 2014; 9(7): 44-46











