What is the evidence for primary tumor and metastasis in breast carcinoma? Are there treatment options that will not harm the child if a pregnant woman is found to have breast carcinoma? From acting without broad evidence in rare situations of breast carcinoma.
(dk) Breast carcinoma exists in many “special situations”, although these are rare (Table 1). For these cases, there are few data from studies, as well as little experience from clinical practice. This fuels uncertainty about how to decide in such situations on a case-by-case basis. Two of these rare situations were addressed by Prof. Jens Huober, MD, Ulm, Germany, at the DESO course in St Gallen: first, primary metastatic breast carcinoma, and second, pregnancy and breast carcinoma.

New study findings from India and Turkey
Primary metastatic breast carcinoma in women is one of these situations rarely covered by randomized trials to date. Approximately 5-10% of primary tumors are already metastatic at diagnosis. The improvement in survival suggested by local therapy from various retrospective studies was probably due to a selection error, Prof. Huober suggested.
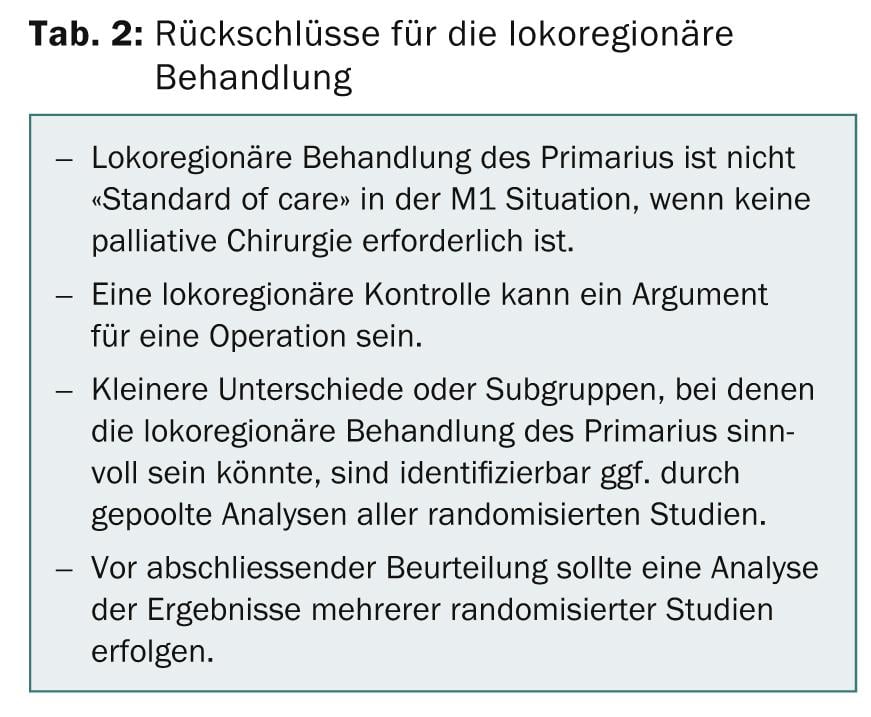
In contrast to these studies, recent data from India and Turkey (Tata Memorial and Turkish Federation Studies) with a randomized trial design show that local therapy of the primary tumor in the M+ setting does not improve survival [1,2]. The design of the MF07-01 trial will randomize Stage IV patients to a systemic therapy only or initial local therapy of the breast and axilla plus systemic therapy group. One endpoint was follow-up to progression, and the primary endpoint was overall survival (OS).
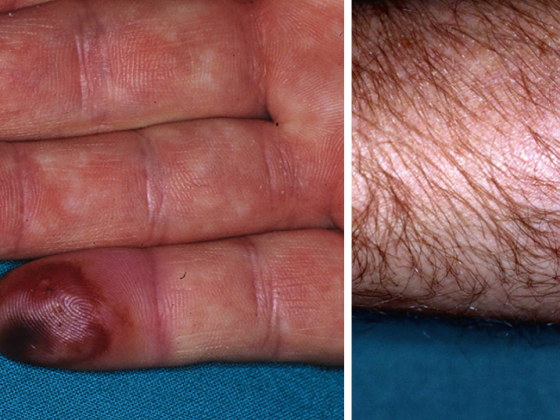
No improved survival was achieved by locoregional therapy of primarius in M+ setting. Subgroup analysis showed a trend for better OS with surgery for bone metastases and patient age greater than 55 years. Poorer OS by local therapy was seen in aggressive phenotypes and multiple liver or lung metastases (Table 2).
Breast cancer in expectant mothers
There was positive news for pregnant women who develop breast cancer. The registry study of the German Breast Group (GBG) has been systematically collecting data of pregnant cancer patients in this regard for years under the leadership of Prof. Dr. med. Sibylle Loib from Neu-Isenburg. Analysis of these data suggests that today, effective therapy and a healthy baby are no longer out of the question [3]. However, Prof. Huober emphasizes that close collaboration with a multidisciplinary tumor center is important because of the lack of experience in treating pregnancy-associated breast carcinoma.
Although the risk of breast cancer decreases with the number of pregnancies, with long breastfeeding periods, and the younger a first-time mother is, breast carcinoma remains the most common malignancy during pregnancy. The older age of first-time mothers also causes a higher number of breast cancers in pregnancy. Here, the symptoms are often confused with the changes of pregnancy. Approximately 2% of all breast cancers are diagnosed during pregnancy. “Unlike years ago, no one today advises pregnant breast cancer patients to abort,” Prof. Huober reported. Current knowledge indicates that prognosis does not improve with termination of pregnancy.
To avoid the excessively high radiation exposure of a mammogram, the lump is usually detected by ultrasound, and a biopsy is then taken to determine whether treatment can be carried out until after the birth. However, data on local therapy from the GBG registry also show that mammary surgery can be performed at any week of pregnancy. Pregnancy is not an indication for mastectomy, and the exact type of surgery is based on the same guidelines as for patients who are not pregnant. “Sentinel node” removal with technetium as a marker is possible, and the threshold dose is low. There is no recommendation for a blue display.
Above all, the placental receptivity of the drugs is the focus of chemotherapy, and bold approaches have already shown that in the second and third trimesters the risk to the child is relatively low. There is little difference in prognosis between pregnant and non-pregnant women with primary breast carcinoma. One recommendation even goes so far as to keep therapy as close as possible to the standard for non-pregnant women. Prof. Huober discussed that “sequence regimens are preferable because of lower toxicity and equal effectiveness, and dosing is based on the woman’s current weight.” Supportive therapy with cortisone and antiemetics, depending on the indication, can be used without risk. It is important to constantly monitor the general development of the fetuses for growth retardation to avoid premature labor. Early delivery should be avoided at all costs because of the increased risk of long-term toxicity and mortality. For delivery, the obstetric situation must be examined. The placenta should be examined for metastases and chemotherapy can be continued one week after birth.
Although breastfeeding is generally possible, it is contraindicated during chemotherapy for up to four weeks after completion of cancer treatment. For this reason, in individual cases, the young mother may well try to pump and discard milk during chemotherapy and then resume breastfeeding.
Source: 24th Physician Continuing Education Course in Clinical Oncology, February 20-22, 2014, St. Gallen, Switzerland.
Literature:
- Badwe R, et al: Surgical removal of primary tumor and axillary lymph nodes in women with metastatic breast cancer at first presentation: A randomized controlled trial. SABCS 2013, Abstract S2-02.
- Soran A, et al: Early follow up of a randomized trial evaluating resection of the primary breast tumor in women presenting with de novo stage IV breast cancer; Turkish study (protocol MF07-01) Abstract S2-03and abstract S2-03.
- Loibl S, et al: Treatment of breast cancer during pregnancy: an observational study. Lancet Oncol 2012; 13: 887-96.
InFo Oncology & Hematology 2014; 2(5): 32-34.