Red eyes are a common reason patients see a doctor. A careful history and assessment of findings are mandatory, but can usually be performed by the primary care physician.
In principle, the following etiologies are possible:
- Sicca syndrome
- Viral or allergic conjunctivitis (conjunctivitis)
- Subconjunctival hemorrhage (hyposphagma)
- Contact lens-associated conjunctival corneal inflammation (keratoconjunctivitis)
- Other causes (foreign body, injury, chemical burn, glaucoma, iritis)
The Sicca Syndrome
Typical of dry eyes (surface moisturization disorder) are chronic symptoms with tearing, itching, foreign body sensation and fluctuations in visual acuity. Clinically, there is redness of the lid edges and conjunctiva. Tear substitutes offer short-term improvement, but in the long term there must always be an evaluation by an ophthalmologist with an accurate determination of the cause. The longer the symptoms persist, the longer it usually takes for the patient to experience definitive improvement from therapy. Humidification disorders increase with age, but can also occur in young patients.
Viral conjunctivitis
Viral conjunctivitis usually manifests as unilateral onset of acute redness of the conjunctiva. The second eye usually follows a few days later. Moisturizing eye drops may be dispensed for symptom relief. The viral inflammation itself cannot be treated. Superinfection by skin germs is not uncommon and manifests as yellowish mucous secretions (Fig. 1).

Therapy for suspected superinfection consists of administration of antibiotic eye drops 3× 1 for five days. Patients are contagious via droplet infection (like a cold). Therefore, people who work in health care, catering establishments, schools, etc. must be on sick leave. As a rule, a patient is no longer contagious after seven days. Hygiene measures are frequent hand washing, the use of your own hand and shower towels as well as your own pillow – and “hands off the eye”! The viruses can survive on door traps or handrails for up to two hours.
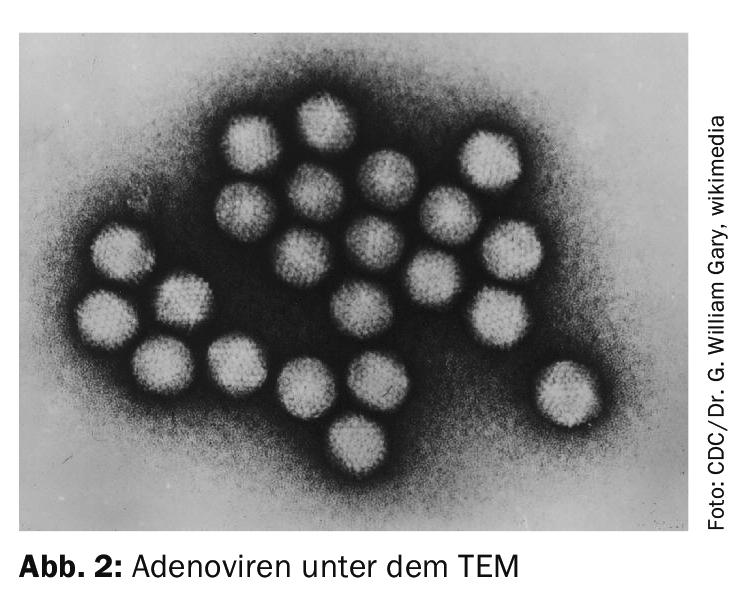
A special form is adenovirus infection (epidemica), a highly contagious, fulminant conjunctivitis. The eye is very red and may show massive conjunctival swelling (chemosis) and persistent corneal opacities. These patients must be evaluated by an ophthalmologist in any case. Patients are unable to work; planned air travel must be postponed because of the risk of infection (Fig. 2).
Typical of herpes viruses are stabbing pain and blinding. For herpes viruses, sometimes topical therapy alone is not sufficient. In this case, the primary care physician and ophthalmologist must discuss together the dosage and duration of peroral antiviral therapy.
Conjunctivitis with allergic etiology
Conjunctivitis is a common side effect of hay fever. It begins bilaterally with redness, tearing and itching. Anti-allergic and moisturizing eye drops can be administered as therapy. Differentiation from viral conjunctivitis can sometimes be made only by slit lamp.
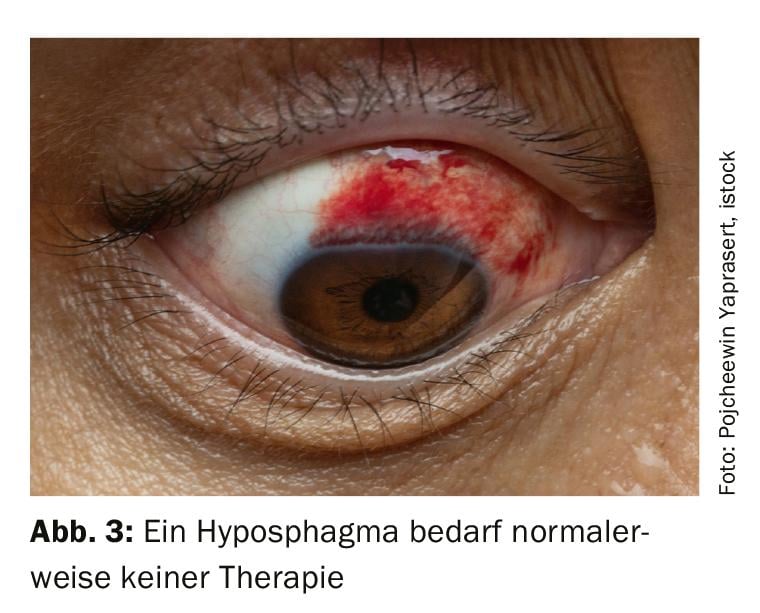
Subconjunctival hemorrhage (hyposphagma)
A ruptured conjunctival vessel can lead to sectorial hemorrhage under the conjunctiva. Visual acuity is not impaired. Therapy is usually not needed; the bleeding reabsorbs over seven to ten days. In cases of recurrent hemorrhage, blood pressure measurement and evaluation by an ophthalmologist with eye pressure measurement is useful (Fig. 3).
Red eye in contact lens wearers
Any inflammatory change in contact lens wearers must be evaluated by an ophthalmologist within 24 hours. Contact lens wearers often have reduced corneal sensitivity and tolerate the lenses even with pre-existing epithelial lesions. Bacterial keratitis can be fulminant and lead to corneal melting and blindness. For a smear test to be successful, no therapy should be started prior to referral. Of course, the patient is no longer allowed to wear the contact lens.
Other causes
Foreign bodies are usually easy to detect. Removal of a conjunctival foreign body can be done using a cotton swab, a corneal foreign body should be removed by an ophthalmologist using a slit lamp, as rust will develop in the cornea within minutes. If the foreign body is not visible, the upper lid must be ectroponed to find a possible subtarsal foreign body. Subtarsal foreign bodies can usually be removed using a cotton swab.
If the patient states that he has come into contact with a corrosive substance, he must urgently rinse the eye thoroughly with water for at least ten minutes. A patient with a chemical burn must be examined by an ophthalmologist.
An acute glaucoma attack results in severe pain, some of which may radiate and clinically mimic a myocardial infarction. The eye is reddened, the bulb is palpatorily rock hard, and the pupil is opaque. Immediate referral to the ophthalmologist is necessary.
Uveitis (iritis) anterior is more difficult to diagnose. Typically, only one eye is affected, the patient reports pain on eye movement and is photophobic. Visual acuity may be reduced. In cases of recurrent uveitis, further search for possible rheumatic diseases is recommended.
Source: Frings A, Geerling G, Schargus M: Red eye – a guide for non-specialists. Dtsch Arztbl Int 2017; 114: 302-312.
FAMILY PRACTICE 2019; 14(8): 30-31