Thoracic pain is a common reason for consultation in the family practice. If an acute coronary syndrome is suspected, the ECG findings, in addition to the clinical presentation and troponin determination, are decisive for the further procedure. Failure to reperfuse patients with ST-segment elevation myocardial infarction (STEMI) within 3-4 hours can have life-threatening consequences.
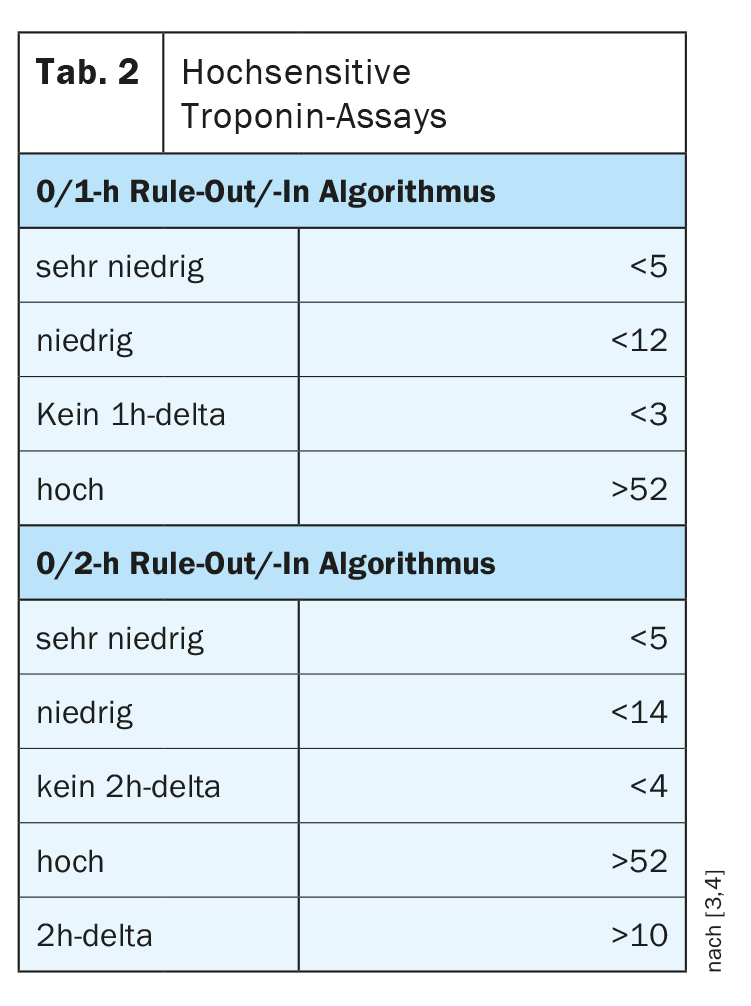
“‘Acute coronary syndrome’ is a collective term for potentially acute life-threatening heart disease caused by a deficiency of blood flow to the myocardium,” says Prof. Christoph Kaiser, MD, Head of Interventional Cardiology, University Hospital Basel [1]. The leading symptom is chest pain. The consequences of acute obstruction of a coronary artery depend on the degree of narrowing, among other factors, and range from unstable angina to non-ST-segment elevation myocardial infarction (NSTEMI) or ST-segment elevation myocardial infarction (STEMI). If the latter is the case, special urgency is required (Table 1).
What are the “red flags” in patients with chest pain?
By definition, the severe thoracic pain in acute coronary syndrome (ACS) persists for more than twenty minutes, possibly with radiation to the left arm, neck, throat, mandibular region. Affected patients should be specifically asked about previous cardiovascular diseases (CHD, st. n. myocardial infarction, TIA or ischemic insult, pAVK). Also important is the assessment of risk factors such as hypertension, diabetes, dyslipidemia, nicotine abuse, and positive family history. Suspicious for ACS in thoracic pain are new symptoms within four weeks, which already occur during light physical exertion such as dressing and undressing, normal walking or light housework, as well as crescendo angina in known CHD with worsening of preexisting symptoms with regard to duration, intensity and frequency. Up to 20% of all myocardial infarctions are silent or present with atypical symptoms such as a feeling of pressure in the epigastrium, nausea, or dyspnea [2]. Indicative of an immediate vital threat with the need for close monitoring are [2]:
- Increasing agitation or disturbance of consciousness (syncope, collapse)
- Respiratory insufficiency (SpO2 <90%), resting dyspnea.
- Signs of acute circulatory failure:
–> Positive shock index: heart rate/BD systolic >1
–> Severe blood pressure dysregulation, hypotension <90 mmHg (forward failure in large anterior wall or right myocardial infarction).
–> Cardiac arrhythmias (ventricular arrhythmias, AV blockages).
- Cold sweating
- Therapy refractory pain
ST elevation on ECG: high probability of STEMI.
“Time is absolutely of the essence in STEMI,” Prof. Kaiser said. “In the first 3-4 hours, you have a big prognostic benefit if you revascularize. Already after 6-7 hours the benefit of such an intervention is only vanishingly small” [1]. If a patient is suspected of having an acute coronary syndrome, an ECG should be performed first. If the ECG shows ST-segment elevation, urgent action is required. With acute chest pain and ST elevation on ECG, the specificity for the presence of ST elevation infarction is greater than 95% and there is no time to lose. Affected patients should undergo reperfusion because a major coronary vessel is occluded. If the findings are normal or without specific changes, i.e., without ST elevation, it is necessary to clarify the possibility of necrosis and to perform a risk stratification with regard to NSTEMI with necrosis vs. unstable angina pectoris without necrosis.
Guidelines recommend highly sensitive troponin assays
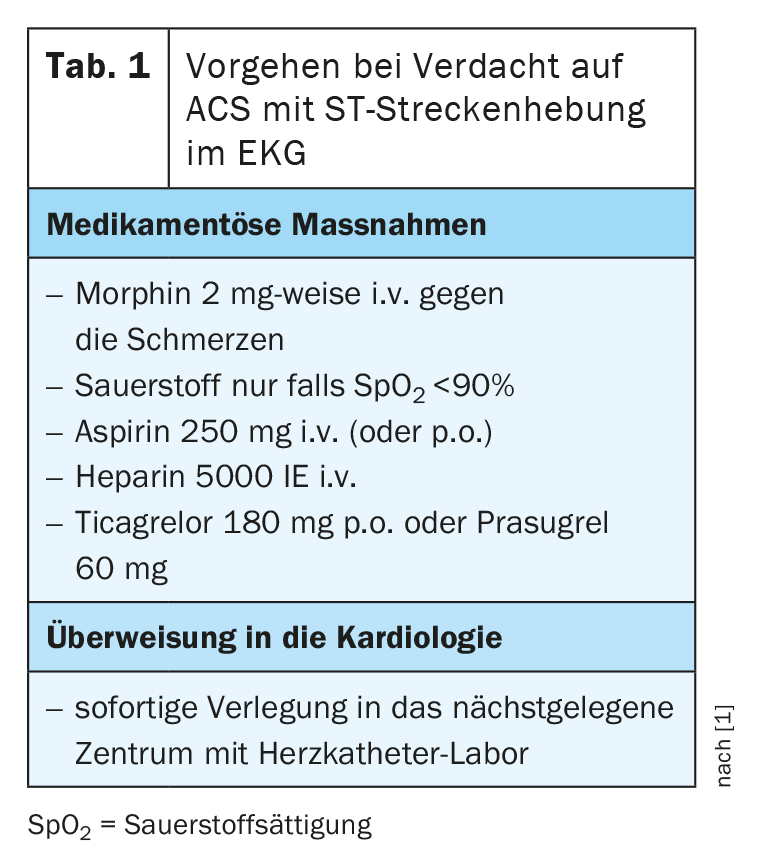
The incidence of STEMI has decreased in recent years thanks to improvements in prophylactic measures. This is also true for unstable angina, whereas NSTEMI prevalence has increased. Prof. Kaiser cites the highly sensitive troponin as the reason for this, which also detects cases that were missed earlier. NSTEMI and STEMI are associated with troponin elevation, whereas angina pectoris is not. According to the 2020 updated ESC NSTEMI guidelines, the use of high-sensitivity troponin tests (hsTn; hscTnI) should be preferred (class I recommendation). If the values in the initial measurement are very low, NSTEMI can be excluded. The 0/1h Rule-Out/-In algorithm is the diagnostic algorithm of choice for ESC. As an alternative, the 0/2h rule-out/-in algorithm can be used. The cut-off values vary slightly depending on the manufacturer, the reference values according to ESC guidelines is shown in Table 2 [3].
Congress: digMedArt21
Literature:
- Kaiser Ch: Acute coronary syndrome, Prof. Christoph Kaiser, MD, digMedArt, 24.06.2021
- Rosemann A: Acute Coronary Syndrome (ACS), mediX-Guideline, 09/2020, www.medix.ch/wissen/guidelines (last accessed 07/16/2021).
- 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal 2020, online August 29, 2020.
- https://doi.org/10.1093/eurheartj/ehaa575
- www.laborchemnitz.de/leistungen/leistungsverzeichnis/detail/leistung/troponin-t-hoch-sensitiv (last call 07/16/2021)
HAUSARZT PRAXIS 2021; 16(8): 28-29 (published 8/18-21, ahead of print).
CARDIOVASC 2021; 20(3): 34-35