A workshop at Medidays in Zurich dealt with the topic of shoulder pain. How can the most common clinical pictures be diagnosed and, above all, differentiated by means of history, inspection, movement tests and imaging? What are the benefits of steroid infiltration? And what options are there for therapy beyond that?
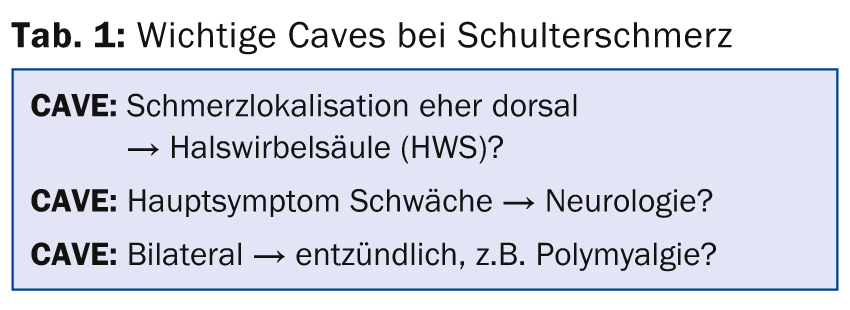
(ag) According to Dr. med. Andreas Krebs of the University Hospital Zurich, not only the medical history but also a good examination technique is crucial for a correct diagnosis. Anamnesis and clinic are indicative for further clarifications and targeted therapy. Exact knowledge of anatomy forms the basis of the clinical examination. They enable precise infiltrations, for example. “The pain localization should be shown. In addition, possible triggers and traumas, movement restrictions, additional symptoms and the presence of night pain or an increase in pain with certain positions or movements should be queried,” says the expert. “The classic location of pain in periarthropathia humeroscapularis is ventral and on the humerus. Inspection includes (comparing the two sides of the body) contours/relief, atrophy, swelling, and movement during clothing removal. Basically, one must always ask and quickly differentiate whether there is an articular or periarticular problem. With free and painless movement in all directions, a shoulder problem is unlikely. Various Caves to Keep in Mind (Tab. 1).”
Active global tests include elevation, apron grip, and neck grip (if smooth, symmetrical, and painless, more relevant shoulder pathology is unlikely).
Passively, articular/capsular mobility and instability can be checked in lateral comparison. You should always start with the healthy side and fix the scapula with one hand at a time (with the patient sitting). Furthermore, selective tests (impingement test best according to Hawkins, tendon test, bodycrosstest for AC joint pathology) are used.
Important differential diagnoses
Differential diagnosis can be made between periarticular pathology (e.g. impingement syndrome, most common cause of shoulder-upper arm pain), adhesive capsulitis (so-called “frozen shoulder”), articular (glenohumeral) pathology such as Omarthrosis, AC joint (e.g. osteoarthritis, arthritis) and special forms such as neuralgic shoulder amyotrophy. The latter is clinically manifested, for example, in acute very intense shoulder pain even at rest and with completely free mobility (pain not dependent on movement). It more commonly affects the right side of the body and is especially seen in younger men. After a few hours to days, pain regurgitation and paresis follow, and later muscle atrophy. Therapeutically, one can only fight the symptoms.
Impingement or “frozen shoulder”?
“The first take-home message is that the so-called ‘frozen shoulder’ primarily restricts external rotation. In impingement syndrome, passive range of motion is better than active, i.e., in painful restricted motion, passive external rotation in adduction reliably discriminates between an impingement and an articular/capsular problem,” Dr. Krebs explained.
Impingement syndrome is a tendon impingement syndrome (most commonly supraspinatus tendon). It originates subacromially and can therefore be treated with subacromial steroid infiltration (40 mg Kenacort® or 7 mg Diprophos®). Peroral medication is usually disappointing and physical therapy is of limited value (for humeral head centering).
Frozen shoulder” is an inflammation of the joint capsule with secondary shrinkage and consecutive stiffening of the shoulder joint. It is associated with pain (also at night) and increasing limitation of movement. The cause is often unclear, primarily it is other pathologies in the shoulder. A “frozen shoulder” can, for example, develop secondarily in the case of a long-lasting impingement symptomatology and thus unnoticed restriction of movement. Therapy initially requires anti-inflammation, preferably with intra-articular steroid infiltration. Only subsequently, i.e. when the inflammation has subsided and the pain has receded into the background, is a slow improvement in movement through physiotherapy useful.
Imaging
Possible avenues of imaging in the shoulder include a conventional radiograph, ultrasound, or arthro-MRI.The conventional radiograph provides information about whether there is omarthrosis, a traumatic lesion, or osseous pathology, and it indicates calcification or narrowing in the subacromial space.
Ultrasound is suitable for detecting an effusion (bursa, glenohumeral, AC), calcification, tendon lesion (in skilled hands sensitivity regarding relevant lesions equal to MRI), and to a limited extent osseous pathology. It can also show the localization for targeted puncture/infiltration.
Arthro-MRI is used preoperatively and provides information about any non-transmural tendon lesion, labral/SLAP lesions (superior labrum from anterior to posterior), and circumscribed cartilage damage.
“The most fruitful additional clarification is ultrasound – the best and most targeted treatment is steroid infiltration. However, with a good indication and an experienced shoulder orthopedist, surgery should not be withheld from older people,” the expert concluded his lecture.
Source: “Shoulder pain in practice”, workshop at Medidays, September 1-5, 2014, Zurich.
HAUSARZT PRAXIS 2014; 9(9): 42-43











