Pseudospondylolisthesis is a form of spondylolisthesis (slipped vertebra). In most cases, a complex degenerative picture of the segmental structures is seen. Foraminal and spinal stenoses are possible consequences of vertebral dislocation. Often the clinical symptoms are heterogeneous and non-specific. In addition to conservative therapy, minimally invasive treatment or surgery can be performed.
Spondylolisthesis is a subluxation of a vertebral body ventrally or dorsally in the next higher segment. Simultaneously, degenerative changes of the intervertebral discs and small vertebral joints are often found. True spondylolisthesis (spondylolisthesis vera, which has already been reported) differs from pseudospondylolisthesis in that there is congenital bony cleft formation in the pars articularis. Ventral vertebral dislocation is usually based on the degenerative changes of the small vertebral joints, preferentially in the L4/5 segment. Disc degeneration is the most common cause of dorsal vertebral displacement, primarily at L3/4 [6,7]. True listhesis is mostly found in the L5/S1 segment with a frequency of 7% of the population [8].
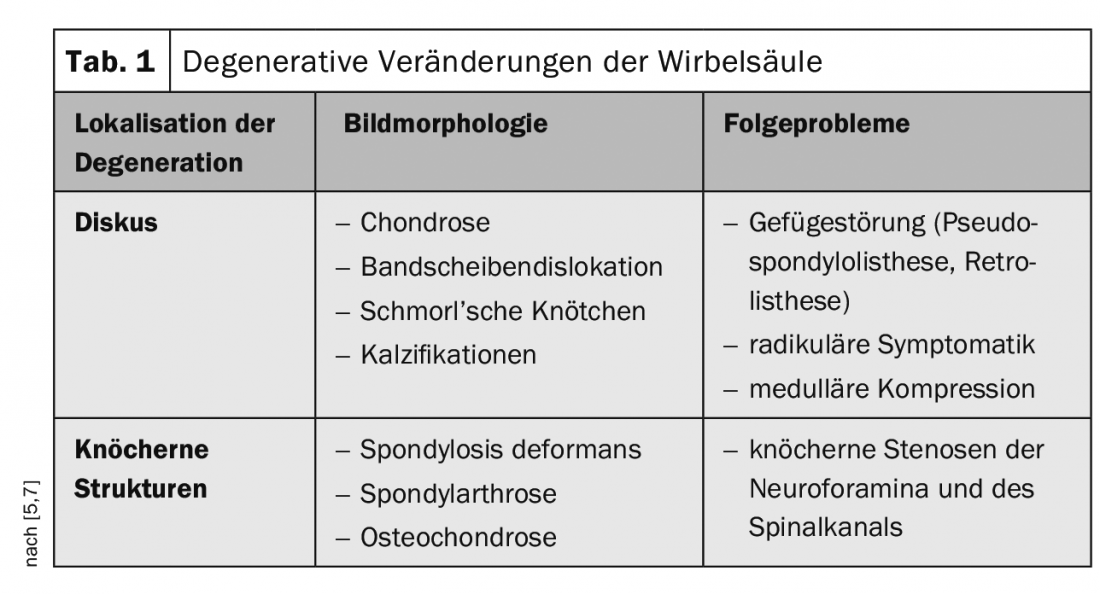
Pseudospondylolisthesis, occasionally described as Junghann’s disease [5], is usually a consequence of degeneration of the spine and offers other aspects of wear in the affected segment in addition to structural disturbance on imaging studies. Table 1 provides an overview.
The clinical symptoms are determined by the back pain, mostly load- or movement-dependent. Pseudoradicular and radicular complaints are possible, paresthesias or blockages. The symptoms are nonspecific, and it is not possible to conclude the cause even by history and clinical examination. Primary conservative therapy includes pain management with medication, physical therapy measures, and, if frustrated, minimally invasive procedures such as CT-guided PRT and/or facet blocks [3]. If the symptomatology is progressive despite treatment and imaging documents a vertebral displacement greater than 50% of the final plate length, neurosurgical consultation is performed. Segmental reduction with interbody fusion raises the prospect of segmental stabilization [4].
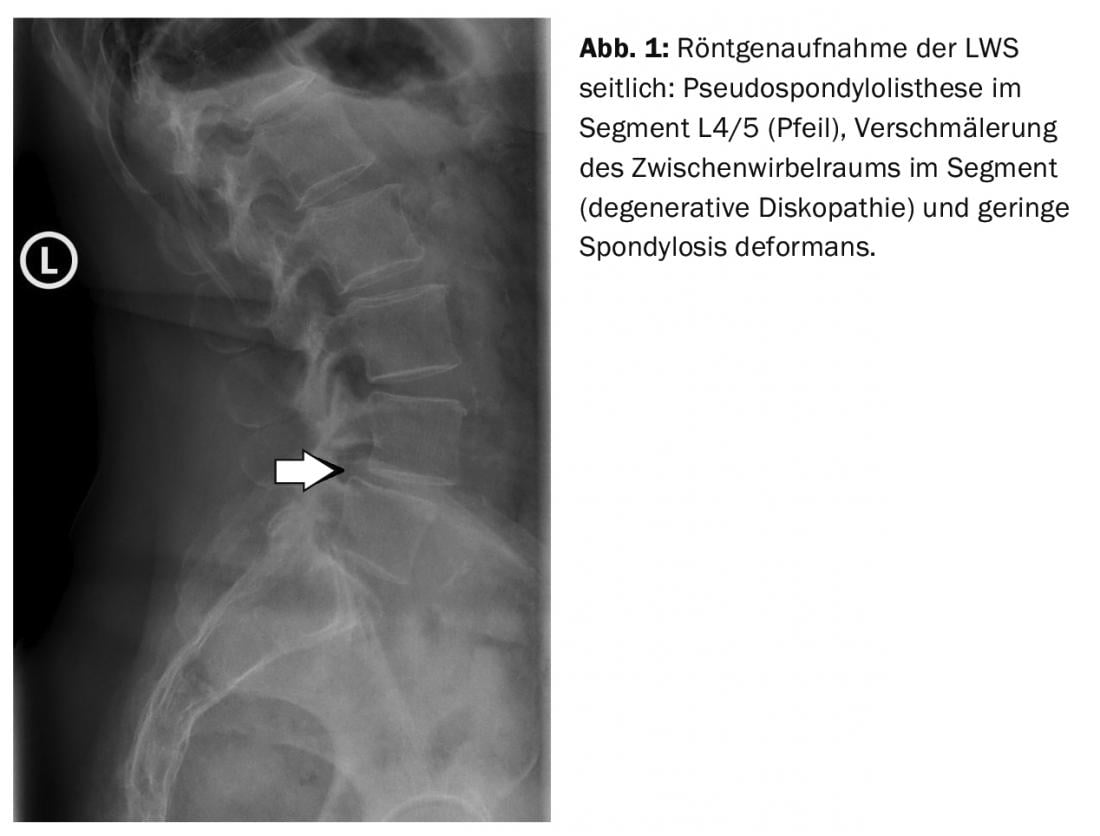
Radiographically, the structural disorder (Fig. 1) is primarily visible in lateral projection. Narrowing of the intervertebral space suggests degenerative discal changes, and spondyloarthrosis can also be assessed.
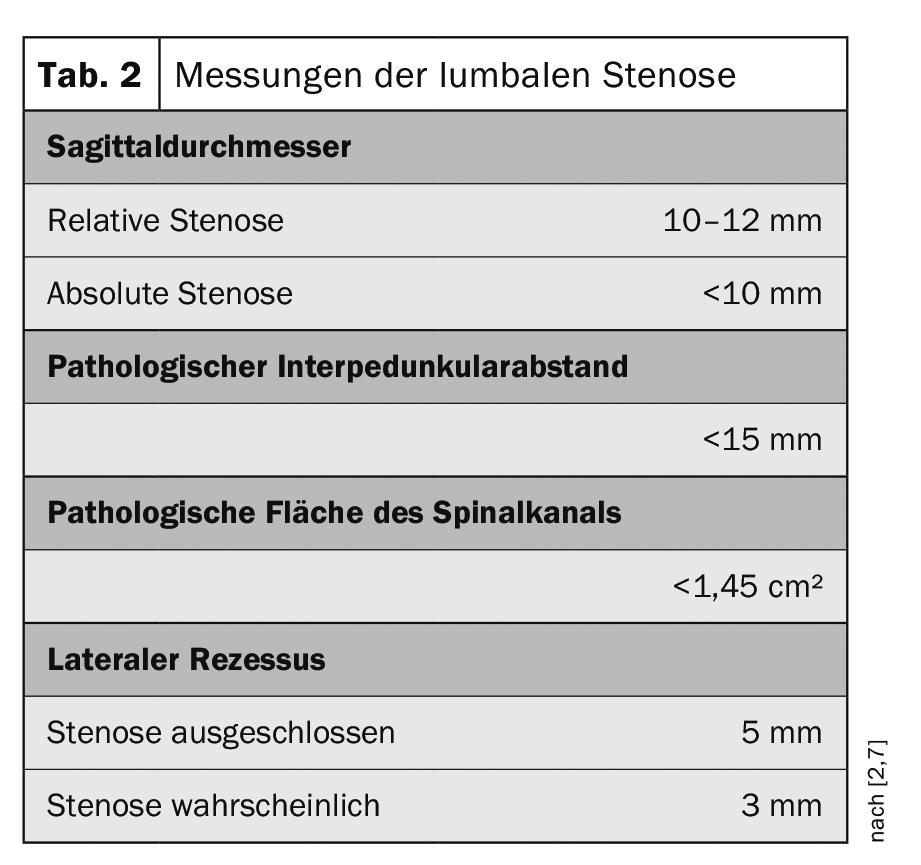
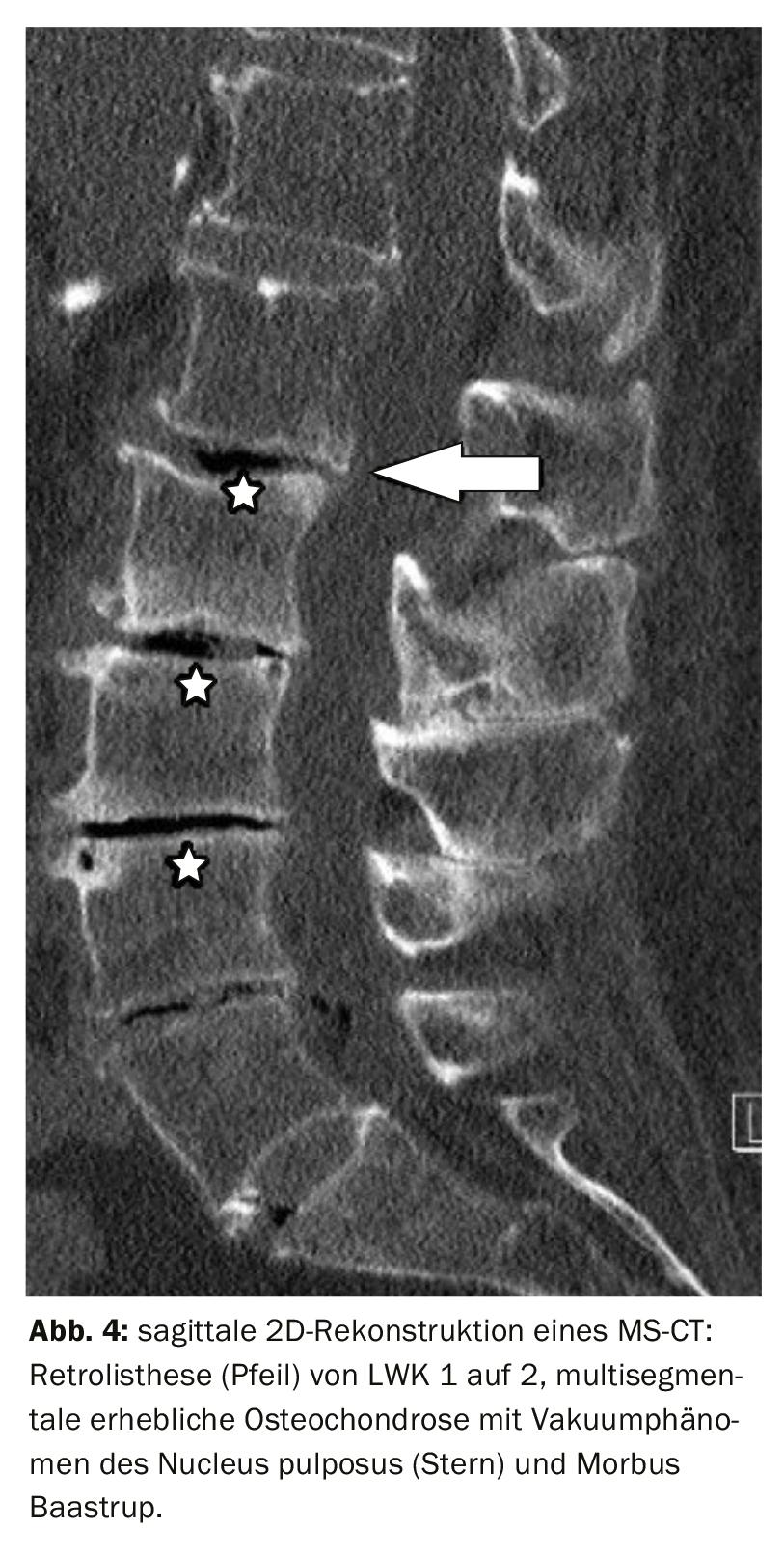
Computed tomographic examinations demonstrate the disruption of the alignment, especially in the sagittal 2D reconstruction (Fig. 4) . A hypertrophic facet joint arthrosis, which can also occur in pseudospondylolisthesis, must be differentiated in the case of increased bone reactions in the bone gap in true lysis with listhesis. Depending on the extent of segmental instability, spinal stenosis may result, which can be very well determined metrically by computed tomography [2] (Table 2).
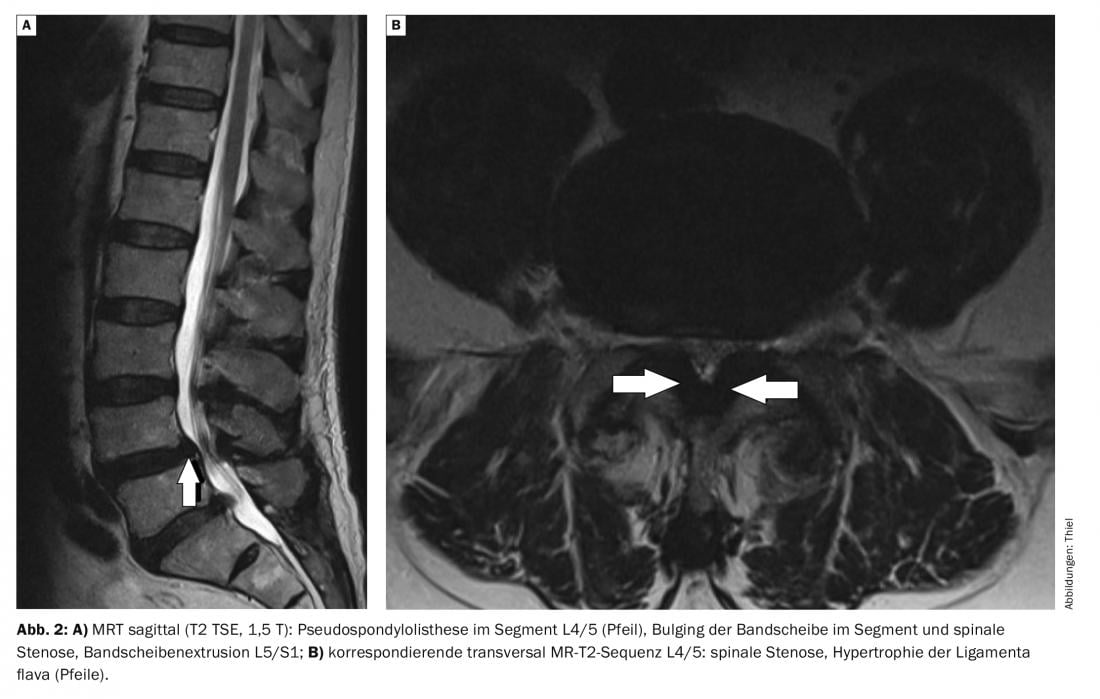
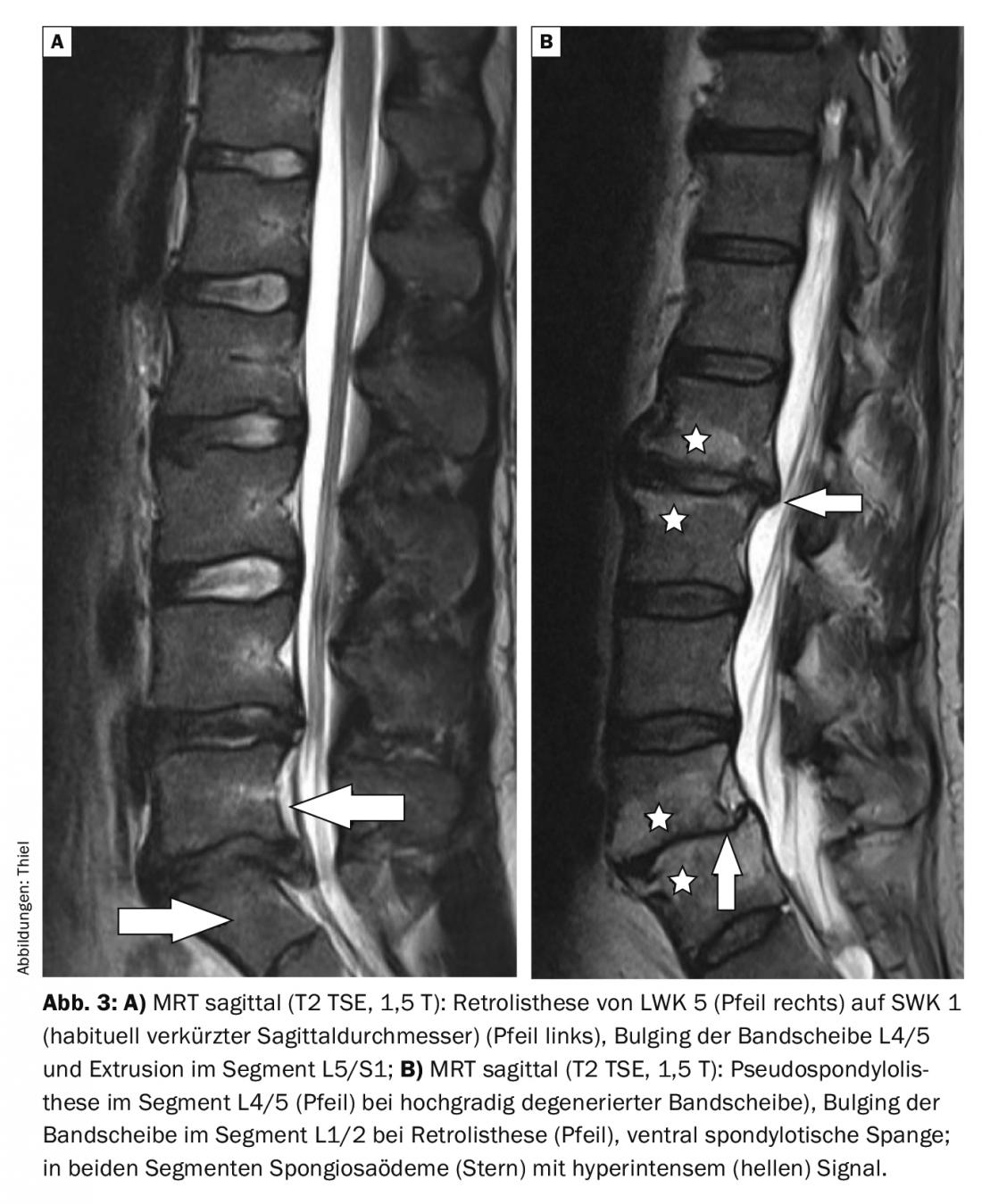
Magnetic resonance imaging (Figs. 2A to 3B) also demonstrates and differentiates true and pseudospondylolisthesis very well [7]. Appropriate mechanical loading and overloading in the segment with instability results in subdiscal spongiosa edema of the vertebrae (Modic 1) with detectable signal changes in the T1w, T2w, and fat suppression sequences [1]. Contrast administration is not obligatory, but would lead to signal increase in the edema zones. The simultaneous frequent irritant effusion in the small vertebral joints is hyperintense in T2w.
Case studies
In the cases presented here, lumbar instability was manifested by back pain, ambulation-dependent leg pain (claudication), accompanied by radiculopathy with motion-dependent lumbalgia. The multiple degenerative changes certainly had an influence on the symptomatology. Neurological deficits with sensory disturbances and paralysis or loss of bladder and rectal continence did not exist. In the case of the concomitant vertebral edema reaction (Modic 1), the lumbalgia intensified with increasing stress during the day.
Take-Home Messages
- Segmental structural disorders of the spine can be caused by spondylolisthesis vera or by pseudospondylolisthesis.
- In pseudospondylolisthesis, a complex degenerative picture of the segmental structures with consecutive spondylolisthesis, disc degeneration and spondylarthrosis/osteochondrosis is usually found.
- Consequences of vertebral dislocation may include foraminal and spinal stenosis.
- Clinical symptoms can provide a “colorful picture” and are nonspecific.
- Depending on the symptoms, treatment is conservative, minimally invasive or surgical.
Literature:
- Burgener FA, et al: Differential diagnostics in MRI. Georg Thieme Verlag: Stuttgart, New York; 2002, pp. 316.
- Grumme T, et al: Cerebral and spinal computed tomography. 3rd, completely revised and expanded edition. Blackwell Wissenschafts-Verlag: Berlin, Vienna; 1998, pp. 246.
- Kalichman L, Hunter DJ: Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J 2008; 17(3): 327-335.
- Kluger P, Weidt F, Puhl W: Spondylolisthesis and pseudospondylolisthesis. Treatment by segmental reposition and interbody fusion with fixateure interne. Orthopaede 1997; 26(9): 790-795.
- Prescher A: Anatomy and pathology of the aging spine. Eur J Radiol. 1998; 27(3): 181-195.
- Rothman SL, et al: Multiplanar CT in the evaluation of degenerative spondylolisthesis. A review of 150 cases. Comput Radiol 1985; 9(4): 223-232.
- Thiel HJ: Sectional imaging of the spine 1.2. Degenerative changes: Pseudospondylolisthesis of the spine. MTA Dialog 2009; 10(3): 182-184.
- Uhlenbrock D, ed.: MRI of the spine and spinal canal. Georg Thieme Verlag, Stuttgart, New York; 2001, pp. 213.
HAUSARZT PRAXIS 2020; 15(9): 47-49