Nodes on the thyroid gland are very common. In the vast majority, thyroid nodules are benign. This is also confirmed by the results of a recent long-term German study, according to which the percentage of nodules that develop into carcinomas is lower than indicated in guidelines. In practice, it is therefore important to avoid over-diagnosis and over-therapy, but on the other hand also to recognize a possible cancer.
After the age of 60, thyroid nodules can be detected in approximately 50% of people [1]. The malignancy rate of thyroid nodules varies widely in the literature, with guidelines reporting values around 5-15% [2,3]. A recent long-term German study on the malignancy risk of thyroid nodules concludes that the numbers are much lower [4,5].
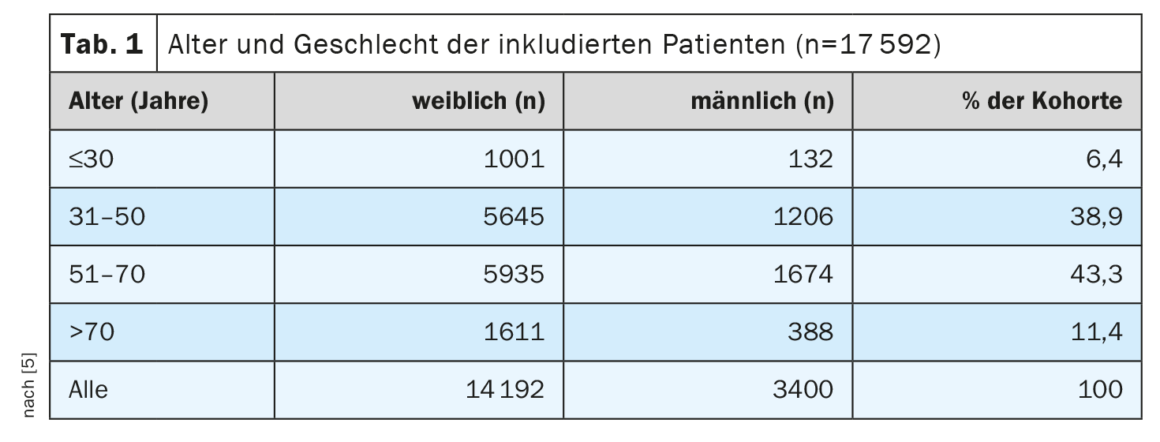
For the analysis, data from more than 17 000 patients were evaluated
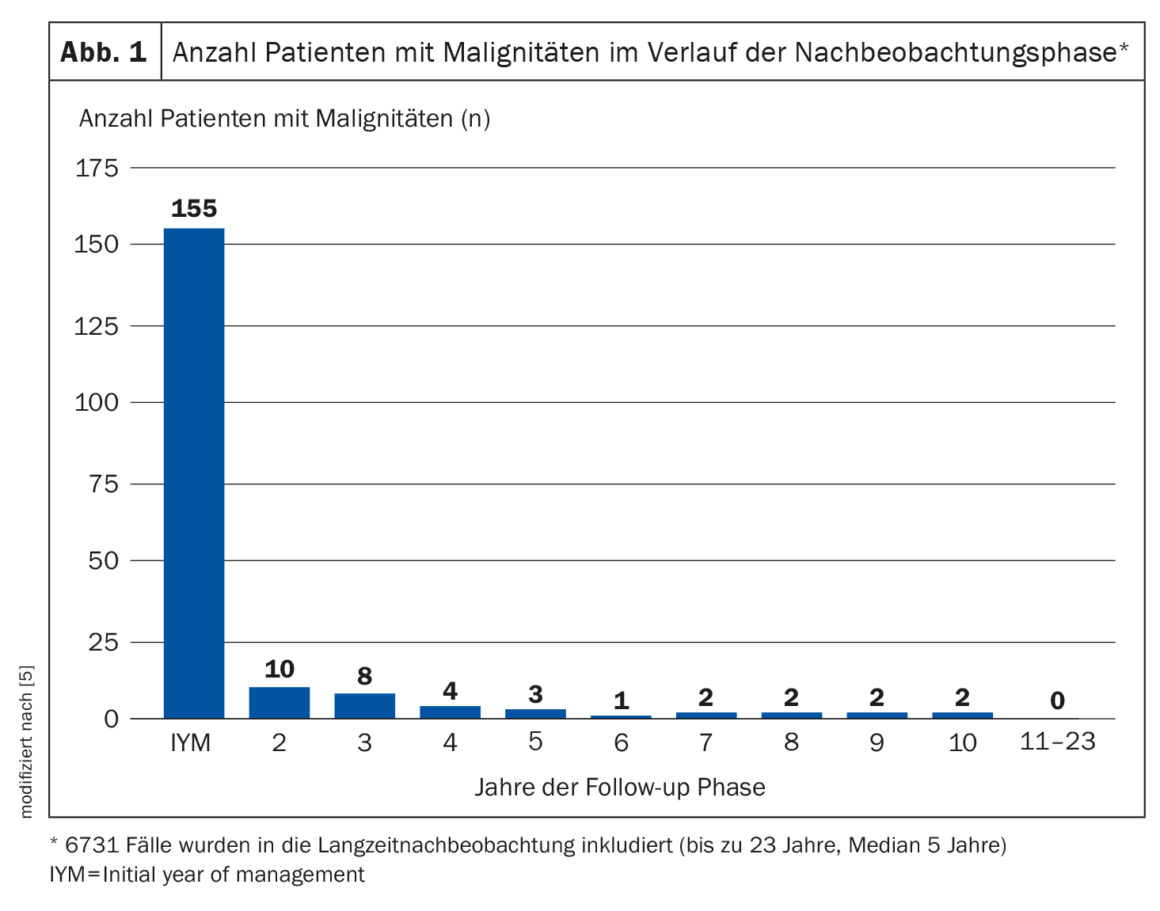
A research group led by Prof. Dr. Martin Grussendorf from the University Hospital Düsseldorf (D) had diagnosed thyroid nodules larger than 1 cm in diameter in 17 592 patients in an endocrinology center between 1989 and 2013 [5]. 9568 patients were initially discharged on the basis of innocuous fine-needle aspiration cytology and/or ultrasound results. Definitive histology was performed in 1904 of the patients, and 6731 cases were included in long-term follow-up (including 1165 longer than 10 years and up to 23 years). In 155 patients, malignancies were detected histologically in the first year after initial presentation, in another 25 a malignancy was detected in years two to five, and in another nine in years six to ten. Thereafter, no further malignant changes were detected until 23 years after initial diagnosis of the nodes. In total, doctors thus diagnosed thyroid cancer in 189 patients. This corresponds to a malignancy rate of 1.1 percent (Fig. 1) .
In what cases is thyroid ultrasonography useful?
To avoid overdiagnosis and overtherapy, the German Society of Endocrinology (DGE) recommends against routine ultrasound screening of the thyroid gland in patients without evidence of thyroid disease [4]. If a nodule > 1 cm in diameter is detected, thyroid ultrasonography with standardized reporting according to TIRADS (Thyroid Imaging And Reporting System) should be performed first. In addition, the professional association advises to determine the TSH value in the blood. If it deviates from the norm, the thyroid hormones fT4 and fT3 should also be measured in the next step. Also recommended is the determination of calcitonin levels. This would allow early detection of the so-called C-cell carcinomas, which occur in about 0.5 percent of cases. Further steps depend on the findings and may include investigations such as fine-needle biopsies and scintigraphies.
Literature:
- Schilddrüsenzentrum Bern, www.schilddruesenzentrum-bern.ch/de/angebot-endokrine-chirurgie/haeufig-gestellte-fragen-zur-schilddruese-faq.html#was-sind-schilddruesenknoten-und-warum-entstehen-sie, (letzter Abruf 09.03.2023)
- Gharib H, et al.: AACE/ACE/AME Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists (AACE), American College of Endocrinology (ACE) and Associazione Medici Endocrinologi (AME) Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules – 2016 Update. Endocr Pract 2016; 22(5): 622–639.
- Haugen BR, et al.: 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016; 26(1): 1–133.
- «Schilddrüsenknoten: Häufigkeit von Schilddrüsenkrebs ist überbewertet – wird zu viel operiert?», DGE e.V, 01.12.2022
- Grussendorf M, Ruschenburg I, Brabant G: Malignancy rates in thyroid nodules: a long-term cohort study of 17,592 patients. Eur Thyroid J 2022; 29; 11(4):e220027. doi: 10.1530/ETJ-22-0027.
HAUSARZT PRAXIS 2023: 18(4): 48
InFo ONKOLOGIE & HÄMATOLOGIE 2023; 11(2): 18