The criteria for cardiovascular risk stratification defined in the current guidelines of the European Society of Cardiology (ESC) form the basis for the calculation of an individual risk score. Non-HDL cholesterol is highly associated with long-term risk of atherosclerosis, new data show. Monitoring and early intervention are critical.
The terms “atherosclerosis” and “arteriosclerosis” are often used interchangeably in clinical usage, although this is not entirely correct. Arteriosclerosis is a collective term for various pathological changes that cause thickening and loss of elasticity of the arterial wall. Atherosclerosis is the most common and clinically significant subtype, as coronary heart disease and cerebrovascular disease are possible outcomes. Atherosclerosis is characterized by atherosclerotic plaques – a vascular lesion composed of lipids, inflammatory and smooth muscle cells, and a connective tissue matrix that may contain thrombi in various stages of organization and calcium deposition. Arteriolosclerosis and primary Mönckeberg-type media calcification are representatives of nonatheromatous arteriosclerosis.
New evidence on the risk factor hypercholisterinemia.
A recent study published in the journal The Lancet demonstrates that non-HDL cholesterol (VLDL*, IDL**, LDL†) is highly associated with long-term risk of atherosclerosis [1]. This underscores the relevance of risk monitoring and intervention measures as early as possible. Based on the Multinational Cardiovascular Risk Consortium, data from 524,444 individuals without manifest cardiovascular disease at baseline, were analyzed. The combined primary end point of atherosclerotic disease was defined as the occurrence of a CHD event or ischemic stroke. Incidence curve analysis shows that the rate of cardiovascular events increases progressively within 30 years as a function of non-HDL cholesterol (in women: 7.7% for non-HDL cholesterol <2.6 mmol/L to 33.7% for ≥5.7 mmol/L; in men: 12.8% to 43.6%; p<0.0001). It also showed that a 50% reduction in non-HDL cholesterol was associated with a reduced risk of a cardiovascular event at age 75 years, with the magnitude of the risk reduction being greater the earlier the cholesterol levels could be reduced.
Cardiovascular disease is the second leading cause of death after cancer in Switzerland [2]. LDL cholesterol (LDL-C) is one of the most important risk factors, with not only the level of LDL-C but also the duration of exposure playing a role. Congenital hypercholesterolemia is associated with a higher risk than a later acquired form. Therefore, the term LDL cholesterol years was introduced in analogy to the “pack years” in smokers [3]. In contrast, the “good cholesterol” HDL correlates negatively with the incidence of atherosclerosis [6], which has been attributed in part to antioxidant and anti-inflammatory properties that contribute to the maintenance of endothelial homeostasis.
The lower the LDL-C, the better
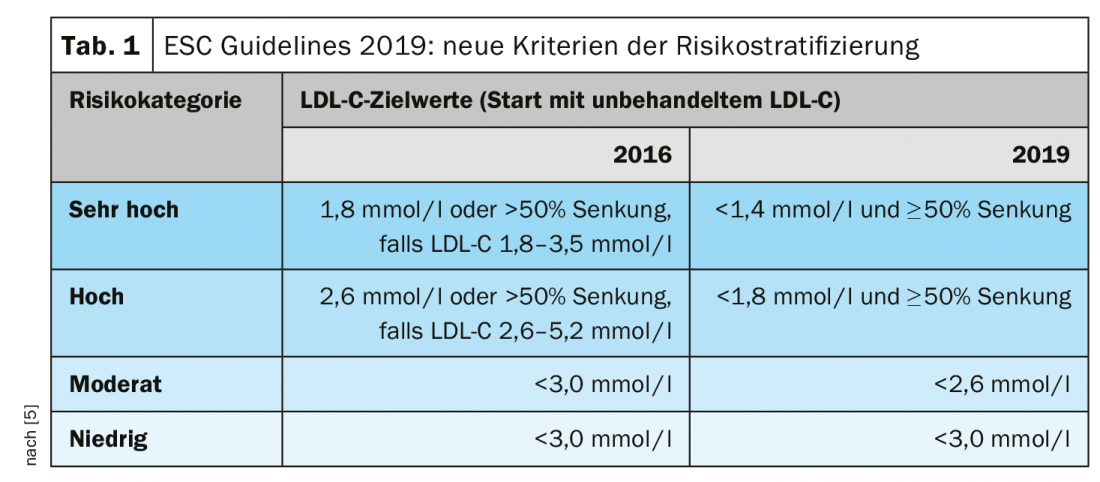
According to the Swiss Working Group on Lipids and Atherosclerosis (AGLA), current knowledge indicates that there is no lower LDL-C concentration limit below which cardiovascular risk does not decrease further. Not only is it beneficial to have LDL cholesterol as low as possible, but also to lower it as early as possible. The current guidelines of the European Society of Cardiology (ESC) [4] also attach great importance to a consistent reduction of LDL-C. Risk stratification based on an estimate of overall cardiovascular risk and the number and severity of risk factors forms the basis for specific recommendations for action. In the updated ESC guidelines published in 2019, among other things, the criteria regarding LDL-C were modified (Tab. 1) . For the estimation of the overall cardiovascular risk, the Working Group on Lipids and Atherosclerosis (AGLA) provides an algorithm specifically adapted to Switzerland [3]. The AGLA Risk Calculator provides a straightforward assessment of overall risk and is available both as a “paper-pencil” version and online www.agla.ch/de/
calculator-and-tools/agla-risk-calculator [3]. Individuals up to 75 years of age can use it to calculate the specific risk of suffering a fatal or nonfatal cardiovascular event within the next 10 years. The AGLA recommendations are based on international guidelines (mainly ESC) and empirical evidence from randomized trials. It is an equivalent to the ESC-SCORE (“Systematic Coronary Risk Estimation”) [3,4]. In contrast to the ESC-SCORE, the AGLA online tool considers not only mortality data but also nonfatal myocardial infarctions [5].
* VLDL = very low density lipoprotein
** IDL = intermediate density lipoprotein
† LDL = low density lipoprotein
# HDL=High density lipoprotein
Literature:
- Brunner FJ, et al: Application of non-HDL cholesterol for population-based cardiovascular risk stratification: results from the Multinational Cardiovascular Risk Consortium. The Lancet 2019 (10215); 394: 2173-2183.
- FSO: Swiss Federal Statistical Office, www.bfs.admin.ch
- AGLA: Lipids and Atherosclerosis Working Group of the Swiss Society of Cardiology (SGK), https://www.agla.ch
- ESC: European Society of Cardiology: 2019 ESC Guidelines Dyslipidaemia (Management of). ESC Clinical Practice Guidelines. www.escardio.org/Guidelines
- Riesen WF, et al: New ESC/EAS dyslipidemia guidelines: an annotated review by the AGLA. Swiss Medical Forum, Online Magazine, 06.01.2020, https://medicalforum.ch
- Ossoli A: Dysfunctional HDL as a Therapeutic Target for Atherosclerosis Prevention. Current Medicinal Chemistry 2019; 26(9): 1610-1630.
GP PRACTICE 2020; 15(6): 46











