High blood pressure is still one of the leading causes of death. Despite good diagnostic possibilities, a large proportion of hypertension patients are not well controlled. That has to change.
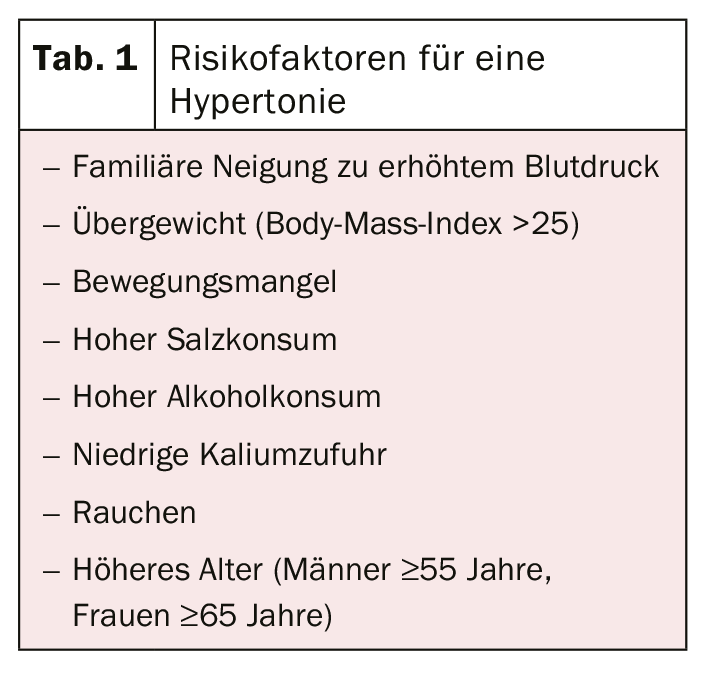
High blood pressure does not hurt. It is not felt and does not cause any discomfort for a long time. Until the consequences such as apoplexy, myocardial infarction, angina pectoris, heart failure or kidney damage can no longer be ignored. Early diagnosis and effective treatment are therefore indicated to reduce the most important risk factor for cardiovascular disease and premature death [1]. It is estimated that one in four adults in Switzerland suffers from arterial hypertension [2]. The spectrum of vascular diseases, which are predominantly triggered by hypertension, is wide and ranges from loss of elasticity and the associated increase in resistance to ischemia. Exactly what causes the disease is not yet fully understood. However, several factors may contribute to its development (Table 1) .
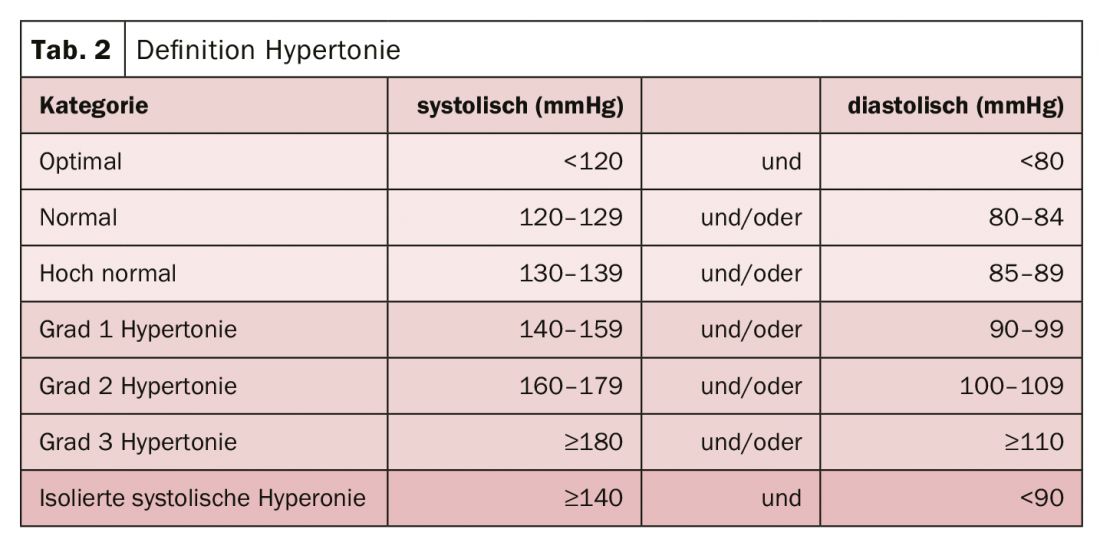
Current guidelines generally recommend initiation of therapy at values ≥140/90 mmHg with a target value <130/80 mmHg (Table 2) [3]. These specifications are independent of possible comorbidities. Only in frail people over 80 years of age should treatment be started only at a value of ≥160/90 mmHg.
Despite a range of therapeutic options, hypertension control is just 50% [4]. The younger the patients, the less well adjusted they are. However, since prevention is always better than cure, greater attention should be paid to individual blood pressure control. Results of a systematic review and meta-analysis demonstrate that as little as a 10 mmHg sBP reduction in blood pressure can reduce the risk of cardiovascular events by 20%, heart failure by 28%, stroke by 27%, coronary artery disease by 17%, and mortality by 13% [5]. There are many reasons for uncontrolled hypertension. Often, treatment options are underutilized. Hypertension is said to be refractory to therapy only when, despite three antihypertensive drugs in optimal dosage incl. diuretic does not reach the target value. This is the case in only about 2% of patients [6].
Reach for combination therapy right away
The maximum response rate to monotherapy is 30-40%. Therefore, the administration of a twofold combination is now also initially propagated. In contrast to dose escalation, the combination is much more effective [7]. The dual combination has an 80% response rate and also strengthens adherence. This is because up to 70% of patients do not take their medication as prescribed. According to studies, the risk of non-adherence increases from the administration of three tablets daily [8,9]. Fixed-dose combinations effectively support the therapeutic regimen in this case.
In the first step, a combination of an ACE inhibitor, renin-angiotensin blocker, or sartan with a calcium antagonist should be resorted to. This was shown to be metabolically advantageous over beta-blockers [10]. The greatest protection against heart failure is promised by the combination of an ACE inhibitor with a diuretic [11]. Beta-blockers should now only be prescribed for specific indications. If no effective blood pressure reduction can be achieved under the two-drug combination at optimal dosage, a switch should be made to a three-drug combination, e.g., ACE inhibitor, calcium antagonist, and diuretic.
Literature:
- https://vizhub.healthdata.org/gbd-compare (last call 01.07.2019)
- www.swissheart.ch/herzkrankheiten-hirnschlag/risikofaktoren/blutdruck.html (last call 01.07.2019)
- Williams B, et al: Eur Heart J 2018. 39: 3021-3104.
- Bundesgesundheitsbl 2013. 56: 795-801.
- Ettehad D, et al: Lancet 2016. 387: 957-967.
- Weitzmann D, et al: Hypertension 2014. 64: 501-507.
- Wald DS, et al: Am J Med 2009. 122: 290-300.
- Strauch B, et al: J Hypertens 2013. 31: 2455-2461.
- Gupta P, et al: Hypertension 2017. 69: 1113-1120.
- Elliott WJ, et al: Lancet 2007. 369: 201-207.
- Sciaretta S, et al: Arch Int Med 2011. 171: 384-394.
CARDIOVASC 2019; 18(4): 22