A research team from the University of Copenhagen conducted a secondary analysis based on data from 72 randomized studies with a total of over 7500 participants to investigate the effectiveness of pharmacological interventions for hand osteoarthritis. The systematic review with network meta-analysis shows that oral non-steroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids are effective analgesic treatment options for osteoarthritis of the hand.
Osteoarthritis (OA) is the most common joint disease worldwide and leads to pain and loss of joint function, especially in advanced stages [1]. Clinically relevant knee, hand and hip osteoarthritis was found in 8.9% of the adult population [2]. Osteoarthritis is characterized by degenerative changes in the joints, which begin with the gradual destruction of the articular cartilage and can lead to the exposure of the bone surface [1]. In addition, the bones, muscles and ligaments adjacent to the affected joints are often damaged. Risk factors for osteoarthritis include older age, female gender and genetic predisposition as well as overloading and incorrect loading of the joints in the case of congenital malalignments (e.g. axial misalignments, hip dysplasia), injuries and accidents, excessive physical activity or inactivity or obesity [1]. Hand osteoarthritis leads to pain, impaired gripping functions and limited mobility, which can have a considerable negative impact on the daily lives of those affected.
Analysis of large databases
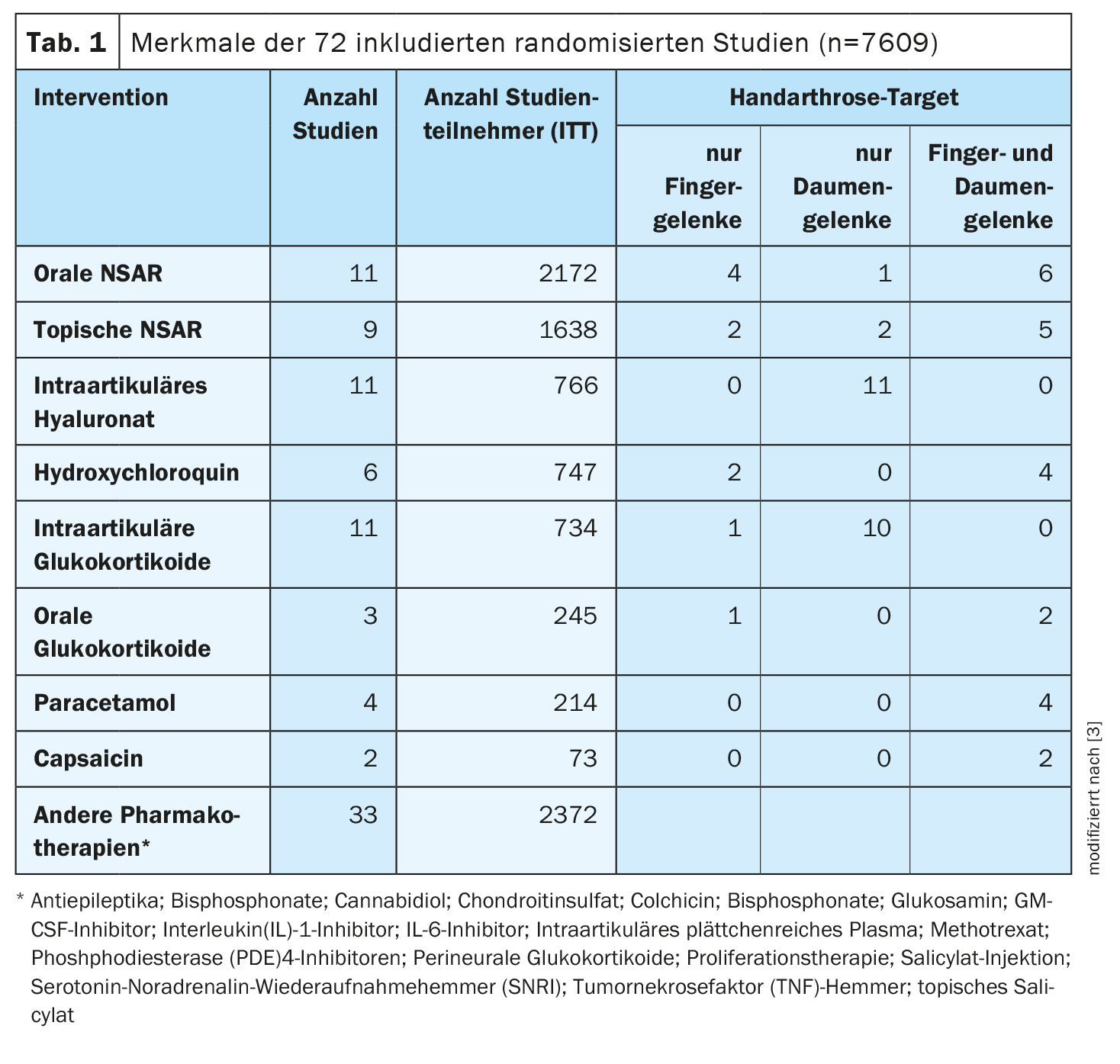
Døssing et al. analyzed data from randomized trials to investigate the efficacy of various pharmacotherapies on the pain symptoms associated with hand osteoarthritis [3]. In addition to pain relief, the effects on functional ability, health-related quality of life, side effects and discontinuation of treatment due to side effects were considered. The researchers used the Embase, MEDLINE and Cochrane Central Register of Controlled Trials databases for their research. Randomized studies up to and including 26.10.2021 in which patients with hand osteoarthritis received drug treatment were considered. From a total of 3319 identified search results, 72 studies with 7609 participants that met the inclusion criteria were initially screened (Table 1) [3]. The requirements for the planned quantitative synthesis were met by 65 of these studies (n=5957), with 29 different pharmacotherapies being used across all these studies. Of the studies included in the quantitative analyses, 60 (n=5246) had pain as an endpoint and were included in the network meta-analysis (NMA); 51 studies (number of participants between 1002 and 4352) were included in the pairwise meta-analysis and 46 (n=4220) in the meta-regression.
Placebo superiority of oral NSAIDs and oral glucocorticoids
Oral non-steroidal anti-inflammatory drugs (NSAIDs) and oral glucocorticoids showed effect sizes of -0.18 (95% confidence interval -0.36 to 0.02) and -0.54 (-0.83 to -0.24) respectively in the NMA in the placebo comparison (Table 2) [3]. This result was consistent when the evidence base was restricted to pairwise meta-analyses of studies without high risk of bias. The effect sizes of intra-articular hyaluronate, intra-articular glucocorticoids, hydroxychloroquine and topical NSAIDs were 0.22 (-0.08 to 0.51), 0.25 (0.00 to 0.51), -0.01 (-0.19 to 0.18), and -0.14 (-0.33 to 0.08), respectively, in the placebo comparison. The treatment effects of oral NSAIDs are supported by consistent evidence of efficacy in the paired meta-analyses, both in terms of pain and functional ability, patient assessment of the disease and grip function. Oral glucocorticoids have also been consistently shown to be effective with regard to these outcome parameters.
Although the long-term safety of the various treatment options was not evaluated in the present analysis, the discontinuation rates due to side effects were calculated. This showed that the rate of discontinuation due to side effects was higher with pharmacotherapeutic treatment than with placebo (Peto OR 1.99; 95% CI 1.41 to 2.82). With regard to the number of adverse events (Peto OR 0.85; 95% CI 0.56 to 1.31), there were no significant differences between the various drug therapies.
According to the authors, the strengths of the study lie in the extensive search strategy, which took into account large databases of relevant studies. As methodological limitations of their secondary analysis, they mention bias risks of some included studies and that the number of included studies and participants was small for certain interventions. With regard to everyday clinical practice, they also point out that the response to treatment can vary depending on whether the osteoarthritis is erosive or inflammatory. It is desirable that more large studies with high-quality evidence on the effectiveness of pharmacotherapeutic interventions for hand osteoarthritis are carried out in the future. There is also a need for better validated questionnaires that differentiate between pain and functional ability in hand osteoarthritis.
Literature:
- Fuchs J, Kuhnert R, Scheidt-Nave C: 12-month prevalence of osteoarthritis in Germany. Journal of Health Monitoring 2017 2(3), DOI 10.17886/RKI-GBE-2017-054, www.rki.de,(last accessed 01.11.2023)
- Andrianakos AA, et al: Prevalence of symptomatic knee, hand and hip osteoarthritis in Greece. TheESORDIG study. J Rheumatology 2006; 33: 2507-2513.
- Døssing A, et al: Comparative effectiveness of pharmacological interventions for hand osteoarthritis: a systematic review and network meta-analysis of randomized trials. RMD Open 2023 Aug; 9(3): e003030.
GP PRACTICE 2023: 18(11): 38-39