Regular medical foot care for people with diabetes can prevent open wounds, infections, and subsequent amputations of toes or the entire foot. However, this had to be done by specially trained personnel in order to be reimbursed by the health insurance company. Now podiatry for diabetes sufferers has been included in health care coverage.
Medical foot care for people with diabetes must be performed by specially qualified professionals on a doctor’s order. Until now, the compulsory health insurance (OKP) only reimbursed this if it was carried out by nursing professionals (Art. 7 Para. 2 let. b para. 10 KLV). However, since many nurses do not have the appropriate experience and equipment, the demand could not be met. Therefore, as of January 1, 2022, medical foot care performed by podiatrists for persons with diabetes will also be reimbursed by the mandatory health care insurance, according to the Federal Council’s communication of May 26, 2021 [2].
Multiprofessional and multifactorial treatment
Among other things, a good “wound network” is needed for multi-professional and multi-factorial treatment by the podiatrist. This includes, above all, cooperation with the physician, who provides information on whether stenoses are present, whether revascularization should take place, and schedules appointments for dressing changes. A nursing service may also be involved for local wound treatment appropriate to the stage. And it requires the help of the patient himself and his relatives, for example, when it comes to hygiene at home or possible transportation services. According to Penelope Kühn, a podiatrist in Nastätten, time also plays a crucial role. This is a great advantage with podiatrists, as they see the patient regularly every 4-6 weeks and have between 30-60 minutes to listen, perceive but also influence [1].
The possible procedure at the podiatrist includes gentle palpation and probing of the wound as well as initial treatment with antiseptic to prevent infection. In addition, there may be direct contact with the primary care physician to clarify competencies. In consultation with the primary care physician, the podiatrist also performs wound or callosite ablation for undermining and provides adequate wound rest and pressure relief with dressings that do not further prevent or interfere with extremity care. This is followed by a consultation with the patient on behavioral measures and an explanation of what restrictions may be necessary to help the wound heal to the extent possible.
Clinical diagnosis is often not sufficient
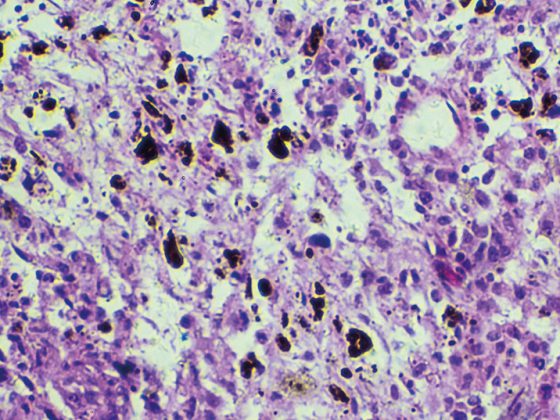
Unfortunately, there are an infinite number of incorrect and false treatments with randomly selected medications, for which there is often no follow-up control as to whether the medication also ensures the desired success, clarifies Ms. Kühn. She therefore recommends that all senses must be sensitized, including in particular looking at, palpating, touching, feeling pressing and smelling. In addition to motor function and sensitivity, regular blood flow monitoring should be performed because in the multifactorial treatment of diabetic foot syndrome, consideration of the arterial blood flow situation is crucial. In addition, in infected patients, pathogen detection should support the diagnosis right at the beginning. However, at the latest when wound healing stagnates, a wound swab should be taken.
The patient remains the focus of the care team. According to Ms. Kühn, in addition to a good and complete medical history, factual communication between all parties involved at eye level is therefore also necessary to ensure good cooperation between doctors, therapists and patients. He said the podiatrist can act as a liaison between the primary care physician and the patient, working with the primary care physician to guide the patient to revascularizing procedures, significantly reducing the risk of amputation.
Case studies from podiatry
Patient A female, 85 years old, diabetes mellitus type 1, ketoacidosis at risk, pAVK, has rubbed his toe on the shoe because the flexor tendon of the toe is much too strong and the extensor tendon cannot really hold against it. This has resulted in an ulcer that has been padded too tightly. The wound was macerated, severely inflamed, had a red coloration and produced secretion. The toe was stretched and the flexor tendon was padded underneath as well as a pad was placed behind the ulcer. High coverage on the actual ulcer should be avoided so that pressure is not transmitted into the wound. Finally, the joint had to be minimally removed and sutured. The wound has now healed and follow-up care is provided using podiatric orthosis to relieve pressure on the toe.
Patient B, male 82 years, diabetes mellitus, PNP, HbA1c level 7.8, pulses palpable, has a metatarsal 5 wound with infection. A wound swab was performed and, with the agreement of the primary care physician, the ulcer was repeatedly opened to allow secretions to drain. The wound was generously padded around the dressing and fixed with Fixomull. As long as the wound is very deep and oozes wound secretions, it must remain open so that the wound secretions can drain off. When padding, the statics and biomechanics should also be kept in mind. Since the statics and dynamics have a great influence on the loading of the forefoot, it is also necessary to look at it from the perspective of spiral dynamics.
Patient C has a wound in the apex area of the D3. Dressing to cover with Fixomull in the flexor tendon was applied in the flexion area. It is important not to glue the pads directly to the skin itself, as the flexor tendon must be prevented from pulling. If the flexor tendon can no longer contract, the toe remains extended and the wound can heal.
Patient D, diabetes mellitus type 2 for 35 years, PNP, physical stiffness, gait unsteadiness and muscle shortening is treated with orthoses. Orthoses are additionally suitable to heal ulcers if close follow-up and good education are provided.
Take-Home Messages
- Different therapists open up different perspectives
- New ideas are developed and reflected
- Structured supply chain
- Important exchange of experience (success & failure)
- The patient with his needs is the focus
- Significantly shorter supply and healing times
- Shorter wound time means lower costs!
Congress: Nuremberg Wound Congress
Literature:
- Penelope Kühn: Pressure ulcer properly relieved and treated in the long term, Nuremberg Wound Congress 2021, 02.12.2021.
- www.diabetesschweiz.ch/mehr-zur-fachberatung/medizinische-fusspflegepodologie.html
HAUSARZT PRAXIS 2022; 17(2): 24-25