At the fourth congress of the Young Family Doctors Switzerland (JHaS) in Thun, Prof. Dr. med. Peter Schmid-Grendelmeier, Head Physician of the Dermatology Clinic at the University Hospital Zurich, spoke about allergies, which are frequently encountered in family practice. Using patient questions, he presented the topic in a practical manner and gave a broad overview of food, insect venom, animal dander and pollen allergies.
(ag) According to Prof. Dr. med. Peter Schmid-Grendelmeier, Head Physician of the Dermatology Clinic at the University Hospital Zurich, respiratory and food allergies in particular are relatively common. Allergies to medications and insect venom, on the other hand, are significantly rarer (Table 1).

The question at the heart of the JHaS congress in Thun was the role of the general practitioner in the overall diagnostic and therapeutic concept of allergies. One thing is certain, the following concerns will be encountered again and again in the family physician’s office:
- I keep sneezing, am I allergic to our neighbors cat?
- I can’t tolerate milk and sausage, nor fruit. Do I have a food allergy?
- Our child has a rash all over his body after a bee sting. Do we need to do something?
- Can my allergy be desensitized?
Diagnosis proceeds by detailed history, clinic, skin tests (in vivo), serological tests (in vitro) and provocation tests.
Knowledge for practice
If one wants to work on the first of the above mentioned cases as a family doctor, one must know for the anamnesis that especially pollen (12-18%) are frequent allergen sources in inhalation allergies. This is followed by house dust mites (3-8%) and animal epithelia (2-9%). 1-5% of the population is allergic to mold spores. In seasonal asthma with rhinoconjunctivitis, particular consideration must be given to the nature of the symptoms, the time of year, weather/place dependence, family and personal history, and evidence of food allergy. Outdoor allergens (such as pollen) lead to seasonal forms, while indoor allergens (such as cat dander) lead to perenneal forms. Pollinosis is triggered by tree, grass or herb pollen, with peak season lasting from about January to June for trees, from about May to September for grasses and from about July to November for herbs. Allergic conjunctivitis involves bilateral ocular symptoms such as severe pruritus, watery secretion, redness and photophobia. In order to evaluate someone who presents to the family physician’s office with the former question, it should be known that allergic conjunctivitis often occurs along with allergic rhinitis (sneezing, nasal obstruction, pruritus, hyposmia, watery rhinorrhea) and is most common in those under thirty years of age and particularly associated with seasonal allergens (i.e., pollen, not cat dander). In 30-40% of patients, allergic rhinitis is accompanied by asthma with irritable cough, tightness, dyspnea on exertion and expiratory stridor.
Prick test and CAP-FEIA
“In practice, a prick test is useful for immediate-type allergies,” Prof. Schmid-Grendelmeier said. If you want to test for a pollen allergy instead of a cat hair allergy in case 1, you should use birch, alder, hazel and ash on trees, a grass mix (rye) on grasses and mugwort and ragweed (ragweed) on herbs. False positive results of this test can generally be obtained with urticaria factitia and with histamine-releasing test substances such as cheese, and false negatives with drug ingestion (antihistamines, psychotropic drugs). To ensure that a false positive test is not performed, NaCl can be counter tested. In the opposite case, histamine can be used.
CAP-FEIA (RAST) is a quantitative in vitro test for over 300 allergens. Strip tests are semi-quantitative with 6-20 allergens/strip. It can be applied depending on the symptoms/allergen group. If you take the IgE value and it is elevated, this does not mean that an allergy is present. “It is true that increasing IgE levels are related to a higher likelihood of clinical symptoms. However, this value never replaces the medical history. Sensitization is not the same as allergy. Only when symptoms are added can an allergy be assumed,” advises Prof. Schmid-Grendelmeier.
Food allergy
Regarding the second case mentioned above, it is necessary to carry out the following useful clarifications in practice:
- Medical history
- Screening test for food allergy (NMA): Fx5 (cow’s milk, egg, soy, peanut, cod, wheat)
- Screening test for inhalant allergies: Sx1 (birch, grasses, mugwort, mite, cat, alternaria).
According to EAACI, among the non-toxic reactions, there is an immunologically induced NMA and a non-immunologically induced food intolerance, the first of which, in turn, may or may not be IgE-mediated (Fig. 1) .
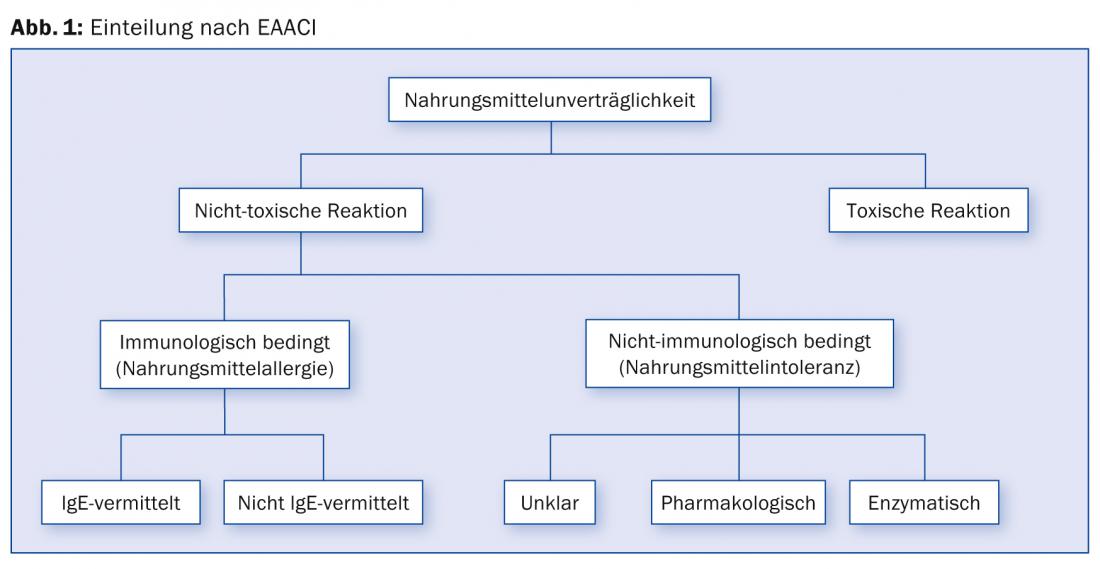
“As a mnemonic, one can say about the immunologically caused NMA: They range from banal to fatal. And for non-immunological food intolerance: Often great agony, rarely for the hospital,” Prof. Schmid-Grendelmeier elaborated.
Symptoms of food allergy predominantly include oral allergy syndrome (OAS), as well as skin, respiratory, and less commonly gastrointestinal and cardiovascular symptoms. IgE-mediated allergic genesis is likely in:
- known inhalation allergy/atopy
- suggestive symptoms for an allergy such as oral pruritus when eating the food and general allergic symptoms (urticaria, asthma, shock)
- Complaints in close temporal relation to food consumption (minutes, few hours).
Some typical cross-reactions are listed in Table 2. For food allergies, a prick-to-prick test can be performed, but care must be taken as anaphylaxis can occur if sensitization is high.

Allergic reactions to insect bites
“One must know that insect venoms (as in case 3), food and drugs are in principle the three most frequent triggers of anaphylaxis. Basically, reactions to stings can be classified according to severity (according to H.L. Müller): Grade I corresponds to urticaria, Grade II to angioedema, vomiting, diarrhea or nausea, Grade III to dyspnea, dysphagia, weakness, drowsiness, cough or stridor, and the last fourth grade to a drop in blood pressure, collapse, loss of consciousness, incontinence and cyanosis,” Prof. Schmid-Grendelmeier explained. A useful measure for the first two degrees is an emergency kit with two tablets of prednisone (glucocorticoid) and two tablets of antihistamine/anti-H1, as well as precise patient instructions for carrying and use. For grades III-IV, the same set plus an epinephrine autoinjector and an allergology workup regarding specific immunotherapy (SIT) is reasonable.
Desensitization
There are two routes of application of SIT: subcutaneous and sublingual. Regarding the effectiveness of SIT, it can generally be said that it is much less effective for food allergies and molds than for mites, feline epithelium or pollinosis. It desensitizes most effectively to hymenopteran venom (hymenoptera).
Complications that can occur during SIT are (in 20-30% of cases) excessive local reactions, which can be addressed by cooling and topical steroids, as well as distribution to both arms or antihistamine protection (1 tbl 1 hour before injection). For the rarer general reactions, one must reduce the dose at least 1-2 levels or possibly consider discontinuation.
“Each patient is instructed about possible allergic reactions and equipped with an emergency kit. In adults, for example, this consists of two tablets of Xyzal® at 5 mg and two tablets of prednisone at 50 mg,” Prof. Schmid-Grendelmeier concluded his presentation.
Source: “Allergien in der Hausarztpraxis – Bewährtes und Neues zu Abklärung und Therapie”, lecture on 4th JHaS Congress, April 5, 2014, Thun
HAUSARZT PRAXIS 2014; 9(6): 42-44