Patients with moderate or severe depression in particular require pharmacologic intervention. Experience shows that antidepressants have their permanent place in the treatment regime of the disease. Selective serotonin reuptake inhibitors (SSRIs) are then primarily used as the drugs of choice. But what if these do not take effect?
Treating depression continues to be a challenge. After classification of the disease and psychoeducation, the decision is made between psychotherapy, medication or both. If psychotherapy can usually be started with mild depression, on the other hand, a combination of both therapy regimes is advisable for severe or chronic depression. But what if the symptoms cannot be alleviated by administration of an antidepressant? In principle, treatment should be adjusted or supplemented if there is no improvement after three to four weeks. Up to 70% of all patients are not in remission even after eight weeks of drug treatment. Just under half still do not, even if the first therapy attempt is extended. First changes should be noticed already within the first 14 days. If this is not the case, a modification of the therapy should be considered.
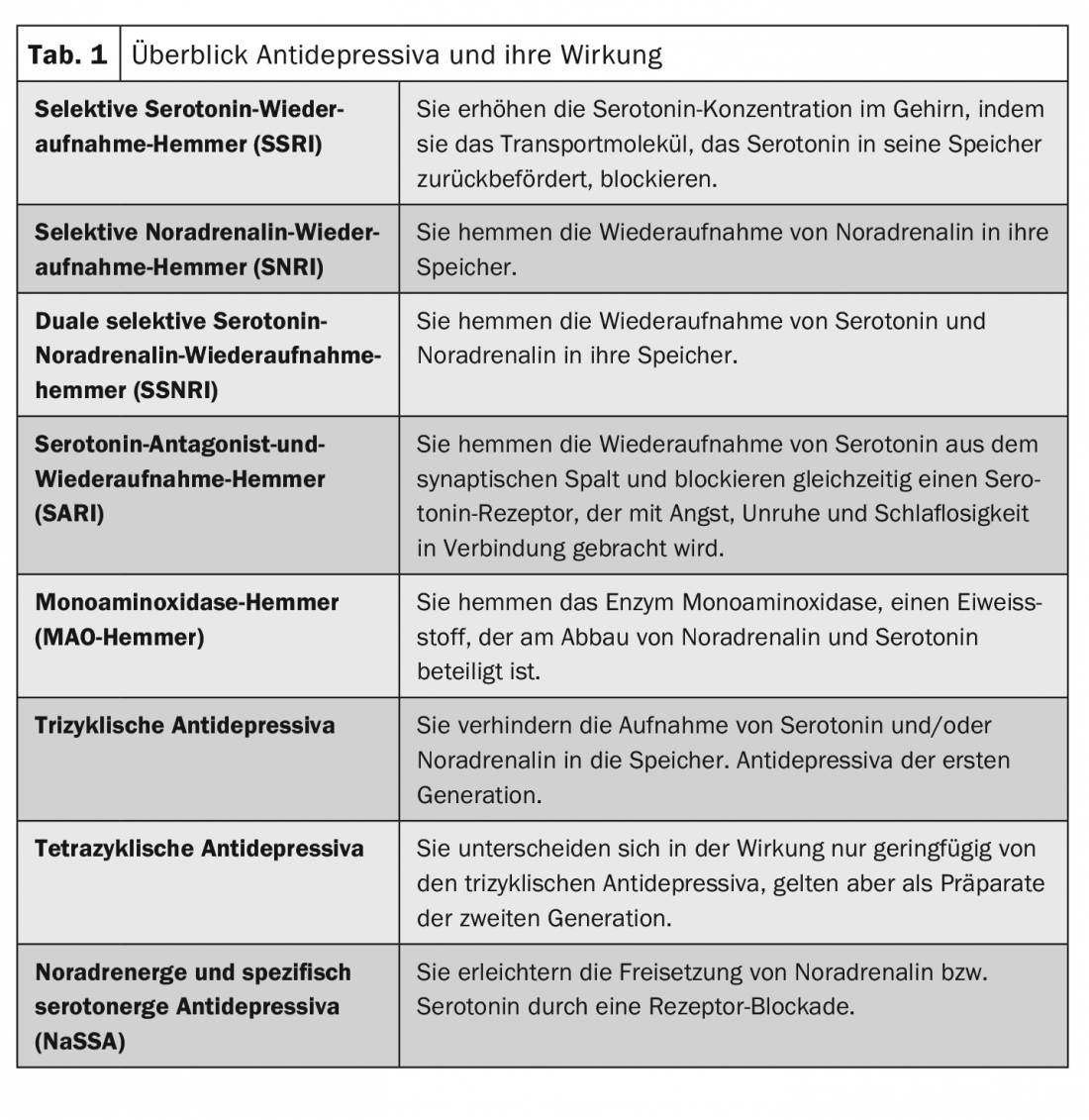
Depending on the preparation, antidepressants have a mood-improving, anxiety-relieving, calming, drive-increasing or drive-dampening effect. Their effect is based on the fact that they make up for the deficiency of the neurotransmitters serotonin and/or norepinephrine. Selective serotonin reuptake inhibitors (SSRIs) are considered the drugs of choice. In addition, there are selective norepinephrine reuptake inhibitors (SNRIs), dual selective serotonin-norepinephrine reuptake inhibitors (SSNRIs), serotonin antagonist-and-reuptake inhibitors (SARIs), noradrenergic and specific serotonergic antidepressants (NaSSAs), monoamine oxidase (MAO) inhibitors, and tri- and tetracyclic antidepressants (Table 1).
If acute therapy is not successful
The general approach is to transition to maintenance therapy for several months after acute therapy. If indicated, recurrence prophylaxis can subsequently be performed for several years. But what can be done if acute therapy does not achieve the desired results? In case of non-response to antidepressant monotherapy despite adequate duration and dose, a choice can be made between different strategies for further treatment:
- Drop
- therapeutic drug monitoring
- Dose increase (not with SSRIs)
- Combination of specific antidepressants
- Augmentation with lithium or a second-generation antipsychotic.
- Switch to a different antidepressant.
Which approach is the right one must be decided on an individual basis. In principle, nonresponse may also indicate low pharmacotherapeutic treatability. Therefore, especially in mild forms, discontinuation of pharmacotherapy should definitely be considered. Further treatment would then be provided via supportive discussions, daily structuring, targeted planning of positive experiences, guided self-help, exercise, awake therapy, or specific psychotherapy. Switching antidepressants is also not a first-line treatment, as no superiority over continuing has been observed to date.
Therapy algorithm promises better results
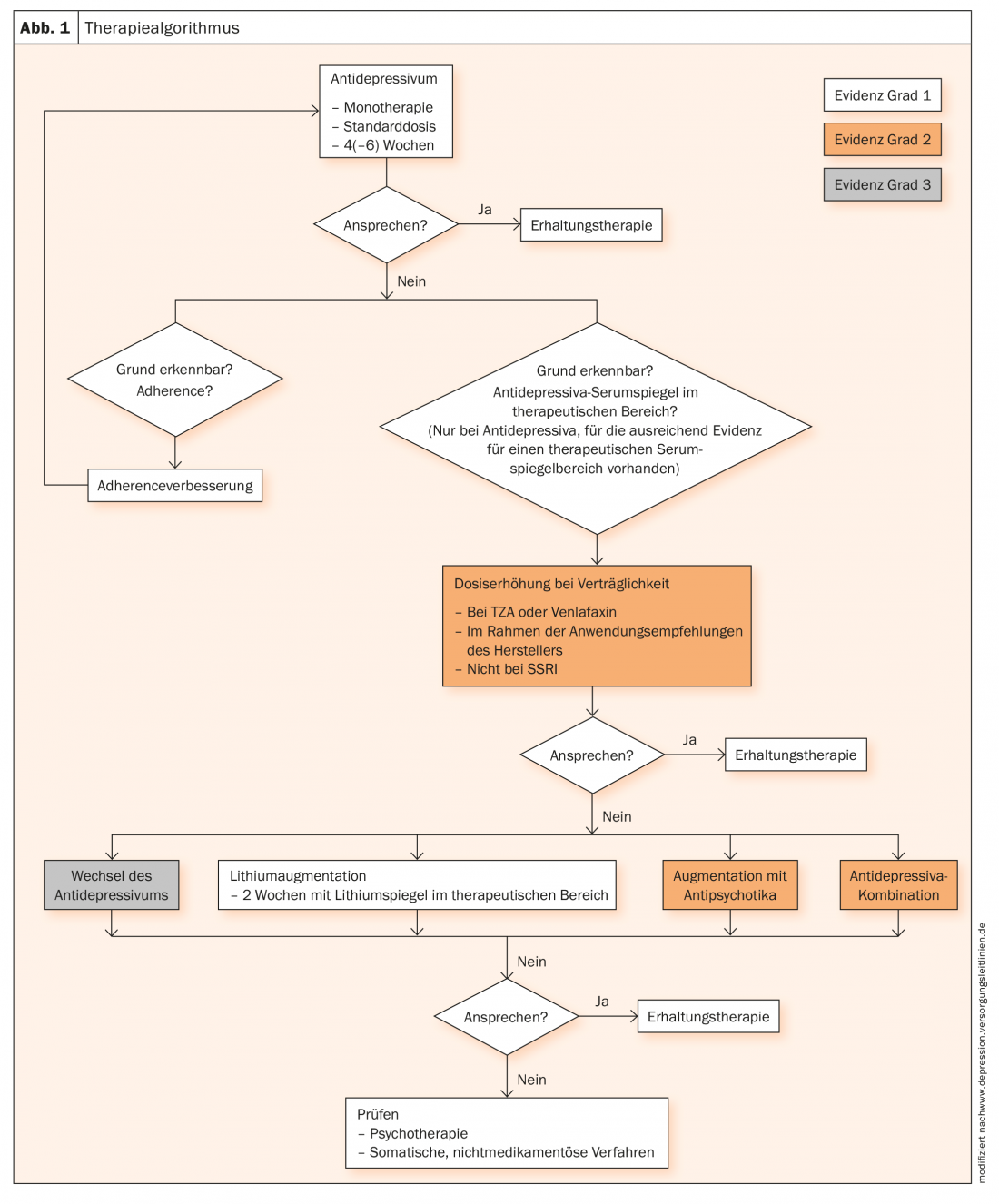
Following an antidepressant stepwise plan is of great importance for the success of pharmacotherapy, as several studies have demonstrated. The central elements of such a treatment algorithm are a clear concept, an appropriate duration of the treatment stages, and a systematic evaluation of the effectiveness at the end of each stage (Fig. 1).
Further reading:
- www.akdae.de/Arzneimitteltherapie/AVP/Artikel/201803/141h/index.php (last accessed 07/28/2020)
- www.therapie.de/psyche/info/index/therapie/psychopharmaka/antidepressiva/ (last accessed 07/28/2020)
- www.neurologen-und-psychiater-im-netz.org/psychiatrie-psychosomatik-psychotherapie/therapie/pharmakotherapie/antidepressiva/ (last accessed 07/28/2020)
- www.psychiatrie.de/psychopharmaka/antidepressiva.html (last accessed 07/28/2020)
InFo NEUROLOGY & PSYCHIATRY 2020; 18(5): 22-24.