An international group of acne experts has analyzed what “gaps” exist in current treatment guidelines and issued new recommendations based on them. There is a focus on a personalized treatment strategy designed to promote adherence in acne patients. Furthermore, long-term management is propagated with the aim of improving the skin appearance of acne in the long term and permanently, thus contributing to an increase in the quality of life of those affected.
Acne, one of the most common dermatologic skin conditions, generally affects adolescents and young adults, but may persist later in life despite treatment [1]. Existing clinical guidelines provide little guidance for personalized and long-term management of acne. Against this background, the international expert panel PACE (“Personalising Acne: Consensus of Experts”) developed consensus-based recommendations using the Delphi method. Most of the 13 dermatologists involved in PACE were co-authors of current European or North American acne guidelines and familiar with the strengths and weaknesses of the respective guidelines.
“Unmet needs” are addressed
Most current acne guidelines are based on clinical trials with a relatively short treatment duration. However, too little attention is paid to various factors, including the following aspects: Trunk acne (affecting more than half of patients with facial involvement), escalation and de-escalation of treatment, maintenance therapy, the patient perspective, and long-term management [2]. Two important “unmet needs” in the management of acne were also identified: first, how to implement a patient-centered treatment strategy in clinical practice, and second, the lack of high-quality evidence regarding long-term maintenance therapy. The latter is associated with a whole bundle of unanswered questions, such as the best time to start therapy, escalation, change of therapy or de-escalation.
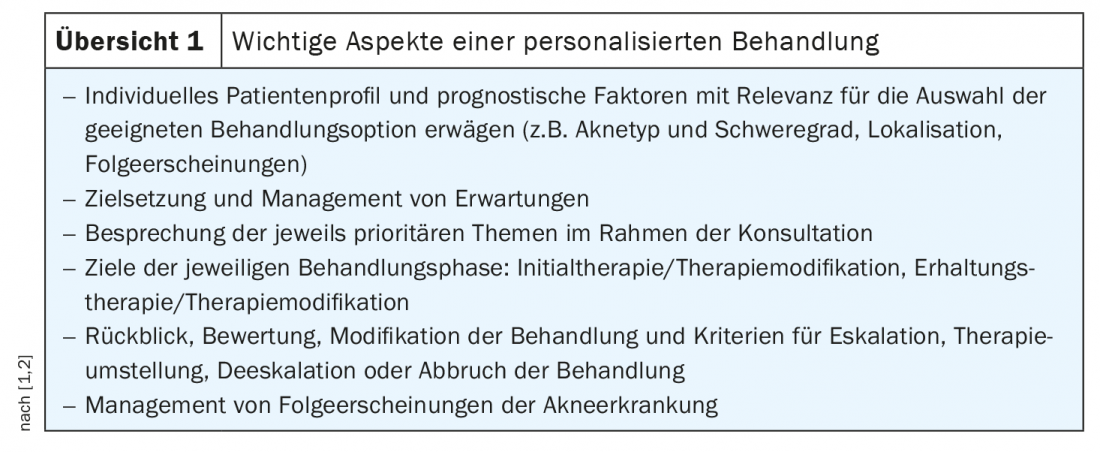
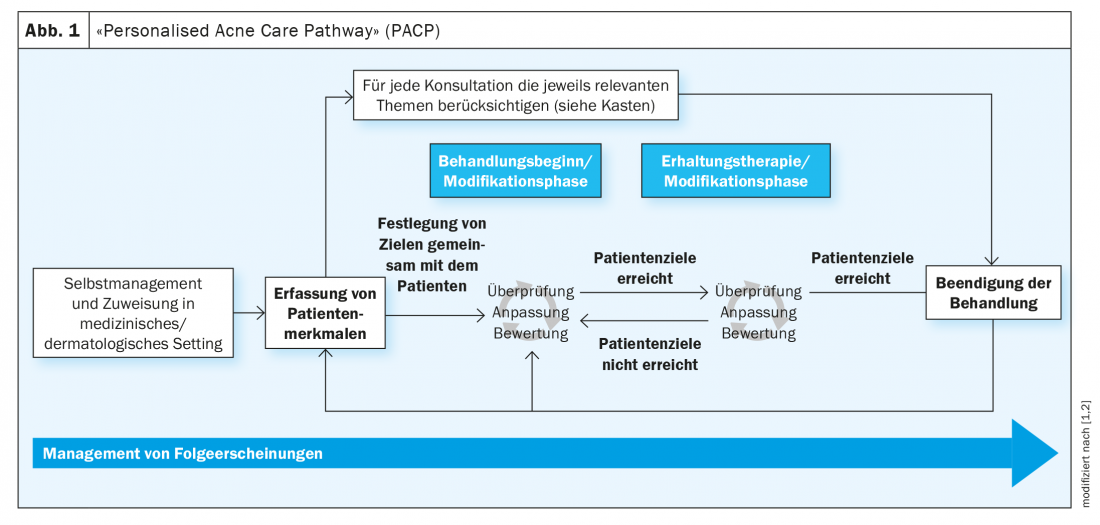
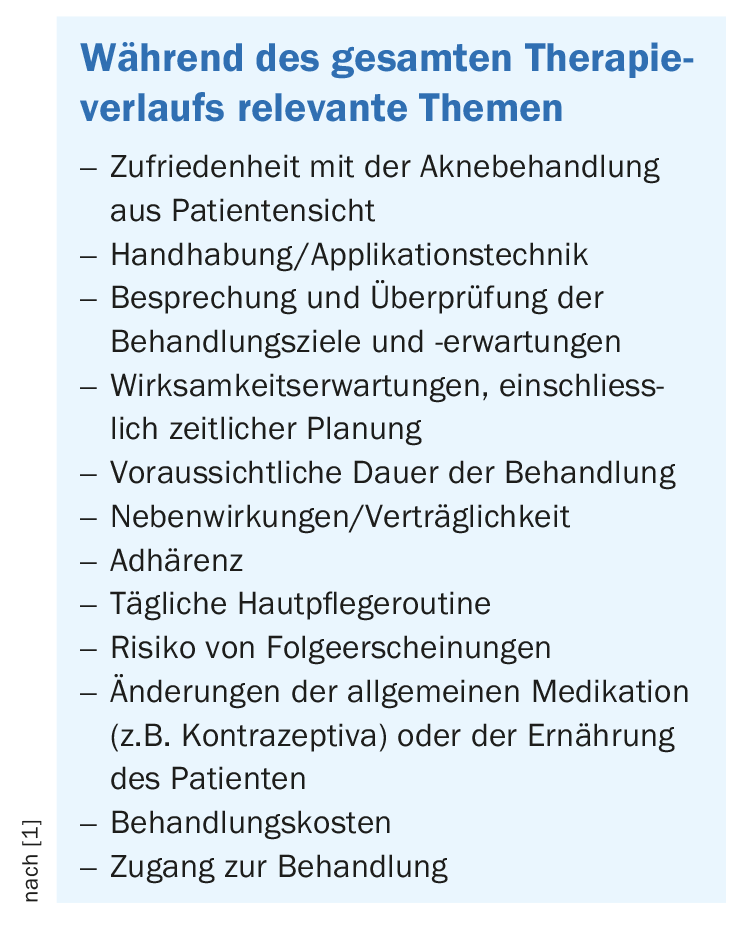
In 2020-2021, the PACE Expert Panel has developed a Personalized Acne Care Pathway (PACP) (Overview 1) to promote comprehensive, personalized, and long-term treatment of acne [1,2]. Part of a patient-centered approach is that treating physicians emphasize discussing expectations for treatment, including timelines and duration of therapy [1,2]. “Topics of conversation to consider at every consultation relate to treatment goals and expectations,” explains Jerry Tan, MD, of the University of Western Ontario, Canada [1]. In particular, the long-term expectations of the therapy should also be taken into account, the expert emphasizes. It is also important to discuss the possible side effects of treatment, the correct use of topical preparations and the adherence to therapy. There was also a strong consensus regarding the requirement that certain subgroups of patients receive special attention. These include patients with dark skin types, elite athletes, transgender patients, as well as pregnant or breastfeeding women, patients with mental disorders, and children under the age of 10.
Personalized treatment strategy and long-term management
It is increasingly recognized that chronic skin diseases, where treatment success is highly dependent on patient adherence, require a personalized approach [3]. Factors influencing adherence include patient characteristics and beliefs, the doctor-patient relationship, and treatment-related factors such as efficacy, side effect profile, tolerability, treatment frequency and duration, and dosage form [4]. In addition, the previous course of the disease and the specific clinical manifestations or localizations play an important role. But access to the health care system (e.g., regarding consultation appointments and treatment costs) also plays a role [4–6]. Low adherence may also be due to lack of response to therapy or low treatment satisfaction. This underscores the need to address patient concerns throughout the treatment continuum and to discuss them in the physician consultation, communicate realistic expectations, and address misunderstandings [7,8].
For the implementation of best-practice recommendations in the long-term management of acne therapy, time, money, and a high level of scientific commitment are needed to ensure that appropriate study projects are funded [2]. Other areas where more research data are needed to provide a better evidence base for treatment recommendations include antibiotic therapy for acne and combination treatments of topicals and oral antibiotics.
Congress: European Academy of Dermatology and Venereology
Literature:
- Tan J, et al: The Personalised Acne Care Pathway. Recommendations to guide longitudinal management from the Personalising Acne: Consensus of Experts, JAAD Int 2021; 5: 101-111.
- Tan J: Optimising longitudinal acne management – recommendations from Personalising Acne: Consensus of Experts (PACE), Presentation ID FC02.01, EADV Annual Meeting, 30/09/2021.
- Abbott P: Patient-centered health care for people with chronic skin conditions. Br J Dermatol 2017; 177(2): 329-330.
- Eicher L, et al: A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease – strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol 2019; 33(12): 2253-2226.
- Poli F, et al: Truncal acne, what do we know? J Eur Acad Dermatol Venereol 2020; 34 (10): 2241-2246.
- Kvarnström K, et al: Barriers and facilitators to medication adherence: a qualitative study with general practitioners. BMJ Open 2018; 8 (1): e015332
- Alsubeeh NA, et al: Treatment adherence among patients with five dermatological diseases and four treatment types – a cross-sectional study. Patient Prefer Adherence 2019; 13: 2029-2038.
- Hayran Y, et al: Factors affecting adherence and patient satisfaction with treatment: a cross-sectional study of 500 patients with acne vulgaris. J Dermatolog Treat 2021; 32(1): 64-69.
DERMATOLOGIE PRAXIS 2022; 32(1): 44-45 (published 9.2.22, ahead of print).