Not only can renal dysfunction be detected by determining glomerular filtration rate (GFR) and albuminuria, but proteinuria in particular is also an early risk indicator for the occurrence of a cardiovascular event. Early detection is an important basis for counteracting cardiovascular diseases through appropriate preventive measures.
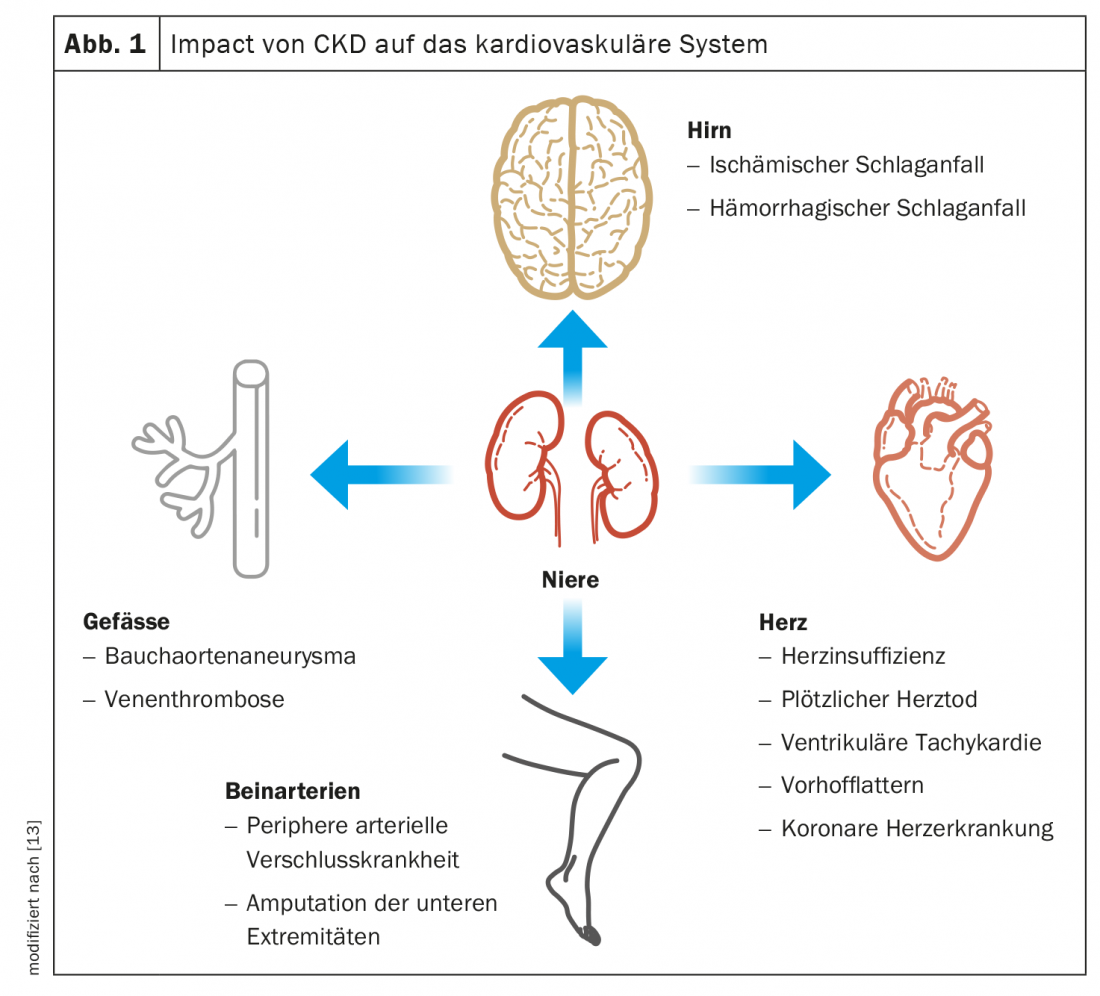
Worldwide, nearly 10% of the population has chronic kidney disease (CKD), defined as a glomerular filtration rate of less than 60 ml/min/1.73m2 and/or a urinary albumin to creatinine ratio greater than 30 mg/g (3 mg/mmol) [1,12]. People with CKD have a much higher risk of cardiovascular disease (Fig. 1) and chronic kidney disease is ultimately also a vascular disease: the glomeruli are made up of tiny clusters of vessels – the kidney function therefore not only indicates the condition of the vessels in the kidneys, but of the entire body. “We can therefore use the kidneys as a seismograph for vascular health, at an early stage, long before kidney failure, a heart attack or a stroke occurs,” explains Prof. Dr. Uwe Heemann, Chief Physician, Nephrology, TU Munich, and adds: “Kidney function is a window to the vessels, but the problem is that we look in far too rarely.” In most people with CKD, it is much more likely that a cardiovascular event will occur than that they will develop end-stage renal disease [12]. A systematic analysis published in 2010 in the renowned journal The Lancet , which included more than 1.2 million patients, showed that simple renal function tests can be used to estimate all-cause and cardiovascular mortality [2].
Early risk assessment recommended
Consistent early detection of kidney disease could thus prevent not only dialysis cases, but also other vascular events such as strokes or heart attacks, which many people fear. The determination of the glomerular filtration rate (GFR) and the collection of albuminuria, two simple and inexpensive laboratory parameters, can therefore be used to assess: What is the condition of the kidneys and the vessels as a whole – and what cardiovascular risk results from this for those affected (box)? “No other procedure provides such an early risk assessment,” Prof. Heemann. However, chronic kidney disease is not only a seismograph for vascular damage, but also its catalyst. A 2018 meta-analysis showed that the typical associated symptoms of chronic kidney disease (CKD), such as elevated serum albumin, phosphate, or uric acid, are independent cardiovascular risk factors [3]. “This also explains why we see a disproportionately high cardiovascular mortality among our kidney patients. While overall about 11% of the population is affected by CKD (all stages), there are relatively few end-stage 5 patients. On the one hand, this is due to successful preventive measures, because we can slow down the progression of kidney disease with medication. Unfortunately, it is also due to the fact that many patients die of cardiovascular diseases before they even reach severe kidney disease requiring dialysis,” states the nephrologist and president of this year’s annual meeting of the German Society of Nephrology. [1,5].
|
Proteinuria as a marker of cardiovascular risk. Chronic kidney disease (CKD) is per se a risk factor for cardiovascular disease, even independently of diabetes mellitus, hypertension, or other known risk factors such as obesity, smoking, or elevated blood lipids [6]. This is especially true if there is an increase in proteinuria [7–10]. Recent data show that the risk of cardiovascular disease correlates more strongly with proteinuria (albuminuria) than with GFR alone. There are empirical findings indicating that when albumin excretion exceeds 300 mg/day, the risk massively increases [11]. Protecting the kidneys is thus also a cardiovascular prevention measure. |
Conclusion
Renal patients are a high-risk cardiovascular population. They require special medical care and should also be educated about their high cardiovascular risk so that they can reduce it by adopting a “more vascular” lifestyle. According to empirical data, male renal patients are at particular risk of stroke and myocardial infarction in middle age. The collection of renal parameters should be routine and integrated into Check-Up 35+ examinations. Early detection of CKD can help identify patients at high cardiovascular risk and direct them to appropriate preventive measures. Regarding drug interventions, for example, it is considered empirically established that SGLT-2 inhibitors have cardiorenal benefits and thus protect the heart and kidney [12].
Literature:
- Briasoulis A, Bakris GL: Curr Cardiol Rep 2013; 15(3): 340.
- Matsushita K, et al; Chronic Kidney Disease Prognosis Consortium. Lancet 2010; 375(9731): 2073-2081.
- Major RW, et al: PLoS One 2018; 13(3):e0192895.
- Alharbi SH: Eur Rev Med Pharmacol Sci 2022; 26(17): 6259-6264.
- “CKD is far more than ‘just’ a kidney problem – kidneys are seismographs for vascular health,” Oct. 07, 2022, German Society of Nephrology (DGfN).
- “Heart and Kidney,” German Society of Nephrology, www.dgfn.eu/hintergrundmaterial.html, (last accessed Oct. 10, 2022).
- Go AS, et al: N Engl J Med 2004; 351: 1296-1305.
- Tonelli M, et al: J Am Soc Nephrol 2006; 17: 2034-2047.
- Hillege HL, et al; for the PREVEND study group. Circulation 2002; 106: 1777-1782.
- Klausen K, et al: Circ 2004; 110: 32-35.
- Astor BC, et al: Am J Epidemiol 2008; 167: 1226-1233.
- Lamprea-Montealegre JA, Shlipak MG, Estrella MM: Heart 2021; 107(16): 1282-1288.
- Mok Y, Ballew SH, Matsushita: Atherosclerosis 2021; 335: 110-118.
HAUSARZT PRAXIS 2022; 17(10): 28-29
CARDIOVASC 2022; 21(4): 34