Atopic dermatitis (AD) is one of the type 2 dominant diseases, caused by complex interactions between genetics and the environment. The role of autoreactive IgE antibodies (auto-IgE) in the pathophysiology of AD has not yet been fully elucidated. In a recent study in AD patients, a correlation of auto-IgE with the presence of comorbidities of the atopic type and with certain environmental factors could be demonstrated.
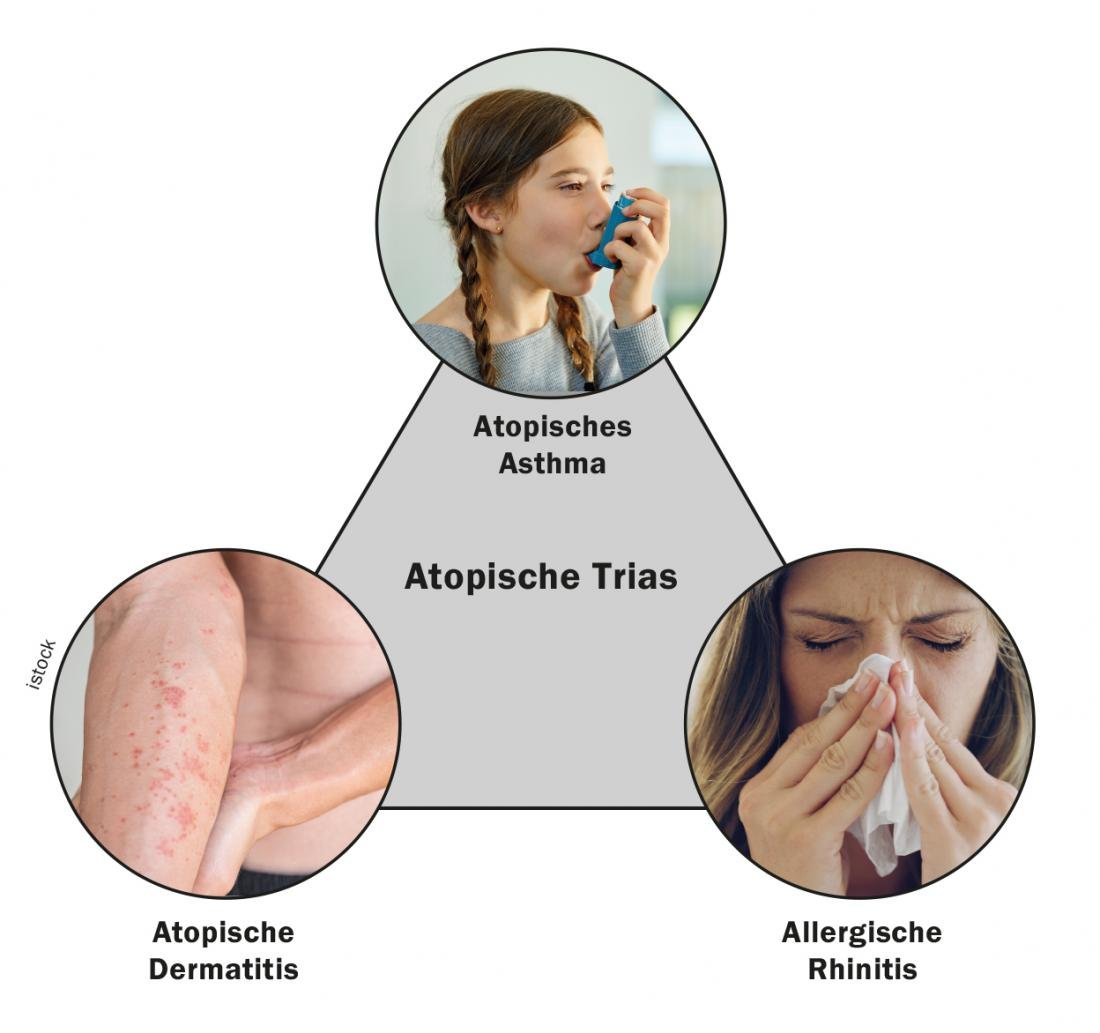
Atopy is defined as a tendency to produce Ig(immunoglobulin)E antibodies in response to low concentrations of allergens [1]. The three classic atopic diseases include asthma, rhinoconjunctivitis, and atopic dermatitis, with IgE-mediated food allergies occasionally included [2]. Atopic dermatitis (AD) often precedes the other atopic diseases, this is illustrated in the concept of “atopic march” [3]. Pathophysiologically, AD is based on complex interactions of genetic factors, barrier defects, a type 2-dominated immune response, and environmental influences [2]. Type 2 inflammation is caused by an exuberant response of the immune system and is a common feature of a number of inflammatory diseases, which include asthma as well as atopic dermatitis [4]. In 50-80% of AD patients, allergen-specific IgE antibodies against aeroallergens or food allergens can be detected.
Data set of the PRORAD CK-CARE study
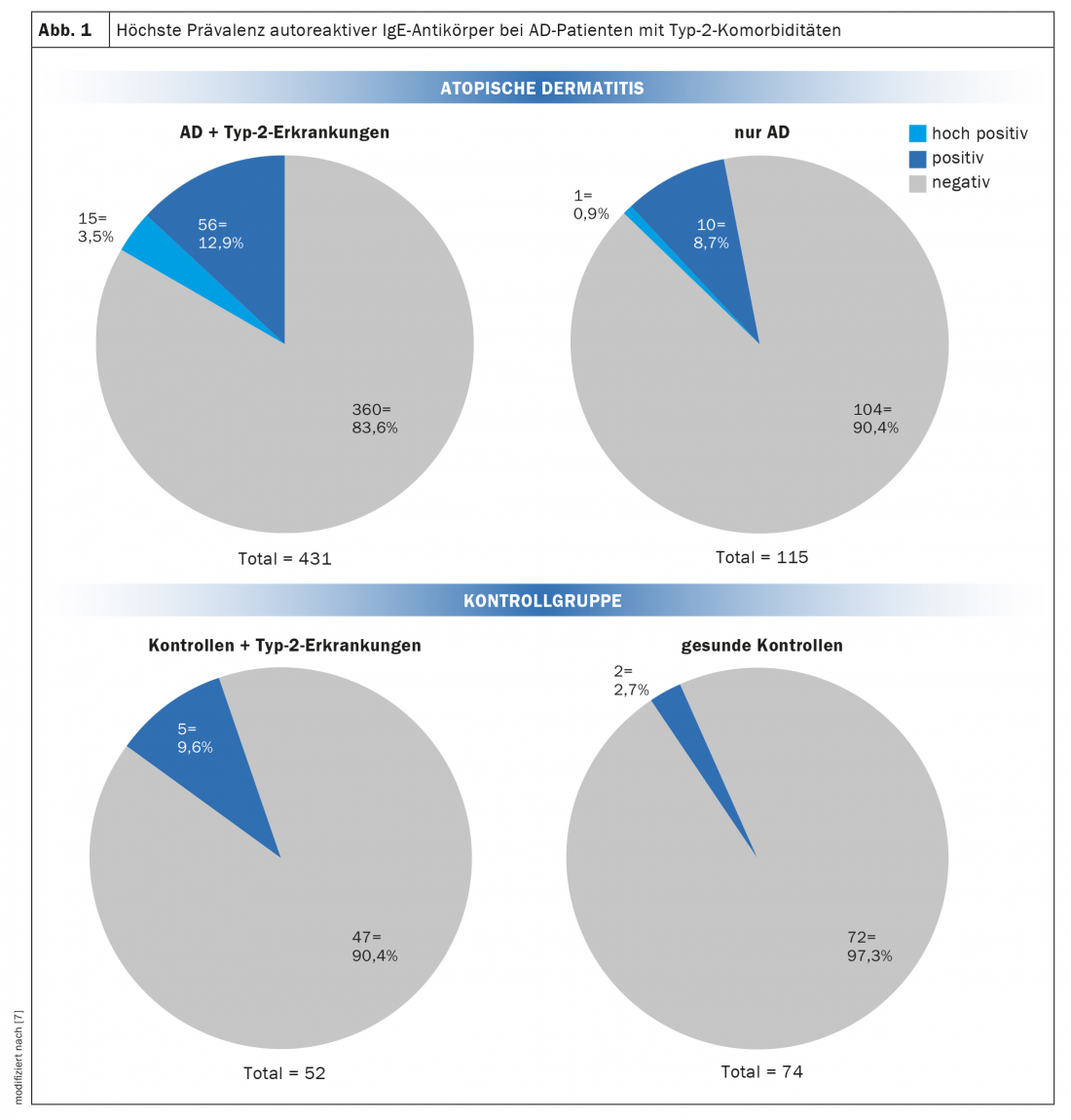
At this year’s Annual Meeting of EEACI (The European Academy of Allergy and Clinical Immunology), a project was presented that aimed to find out more about autoreactive IgE antibodies ( auto-IgE) in atopic dermatitis using data from the PRORAD CK-CARE study ( box ) [6,7]. Previous studies have identified auto-IgE directed against self-epitopes in the skin in patients with atopic dermatitis (AD). However, their importance in the pathogenesis of AD has not yet been elucidated. There is a lack of information regarding prevalence, and on possible risk factors leading to IgE autoreactivity. Also, little is known about correlations to other atopic diseases. In the present study, serum samples from a cohort of well-characterized AD patients and controls were tested for auto-reactive IgE antibodies. A total of 547 patients with AD were included, divided into two groups; within the control group, two groups were also formed:
- AD+type2: atopic dermatitis plus type 2 diseases (asthma, allergic rhinitis, food allergy): n=431
- AD only: atopic dermatitis only: n=115
- Controls + type 2 disease: n=52
- healthy controls: n=74
| The PRORAD CK-CARE study is a prospective longitudinal study to investigate the remission phase in patients with atopic dermatitis (AD) and other allergy-associated diseases such as asthma, food allergy, and allergic rhinitis [6]. The goals of the study are to better understand the mechanisms influencing the course of AD and allergic comorbidities, to better characterize the broad clinical spectrum, to identify clinically relevant and validated biomarkers, and to develop new approaches for the prevention and treatment of atopic dermatitis and associated diseases. |
IgE autoantibodies as biomarkers for progression prognosis?
Analyses were performed using an immunoassay with proteins derived from primary human keratinocytes. The results are shown in Figure 1. IgE autoantibodies were found in 16.4% of AD+type2 patients (15 highly positive, 56 positive, and 360 negative), whereas in AD-only patients, 9.6% had positive IgE autoantibodies (1 highly positive, 10 positive, and 104 negative) [7]. Among the patients with high IgE autoantibody levels, 15 of 16 were AD+type2 patients. Of controls+type2, 9.6% were positive, whereas 2.7% were positive in healthy controls.
Interestingly, AD+type2 patients born between January and May are more likely to develop IgE autoantibodies than those born between June and December, or compared with AD-only patients and controls.
Among AD patients, about 30% of auto IgE-positive patients did not have a pet, compared with 11% of auto IgE-negative patients. Controls showed a similar picture (29% vs. 6%). This observation is consistent with the hygiene hypothesis discussed in the context of allergy-associated diseases. Further, the investigators found that early disease onset was associated with the development of type 2 comorbidities, but not with the development of IgE autoantibodies. Total serum IgE was higher in patients with AD+type2 disease than in AD-only patients or controls, whereas no association with IgE autoantibodies was detected. Overall, the results reflect a strong correlation between IgE-mediated autoreactivity in the presence of AD in combination with type 2 disease. In patients with AD, IgE autoantibodies could potentially serve as biomarkers for predicting the development of comorbid type 2 disease, the authors said.
Congress: EEACI Annual Meeting
Literature:
- Traidl S, Werfel T: Atopic dermatitis and internal medicine comorbidities. The Internist 2019; 60: 792-798.
- Traidl S, Werfel T: Allergen immunotherapy in atopic dermatitis [Allergen immunotherapy for atopic dermatitis]. Dermatologist 2021; 72(12): 1103-1112.
- Paller AS, et al: The atopic march and atopic multimorbidity: many trajectories, many pathways. J Allergy Clin Immunol 2019; 143: 46-55.
- Ludger K, et al: Type 2 inflammation: place of different biologics in practice. Dtsch Arztebl 2021; 118(50): [20]; DOI: 10.3238/PersPneumo.2021.12.17.05
- Guideline Neurodermatitis, development level: S2k, AWMF register number: 013-02, www.awmf.org/uploads/tx_szleitlinien/013-027l_S2k_Neurodermitis_2020-06-abgelaufen.pdf, (last accessed 07/01/2022).
- ProRaD study: prospective longitudinal study to investigate the remission phase in patients with atopic dermatitis (AD) and other allergy-associated diseases such as asthma, food allergy, and allergic rhinitis, https://ck-care.ch/studien/pro-rad-studie, (last accessed 07/01/2022).
- Badloe F: Autoreactive IgE antibodies in atopic dermatitis are associated with Type-2 diseases and environmental factors, Flash Talks on atopic dermatitis and environment, 001508, EEACI Annual Congress, 07/01/2022.
DERMATOLOGIE PRAXIS 2022; 32(4): 22-23