Also known as Sneddon-Wilkinson syndrome, this rare disorder is characterized by primary pustular changes predominantly in the trunk and proximal extremities. Histopathologic examination complementary to physical inspection and history allows differential diagnosis. Dapsone is considered a proven treatment option, in addition to several other treatment options.
Subcorneal pustular dermatosis was first described by Lan Sneddon and Darell Wilkinson in 1956 [1]. It is a chronic but benign inflammatory neutrophilic dermatosis that is four times more common in women than in men [2]. It typically affects middle-aged patients, but some cases have been reported in children. Little is known to date about etiology and pathophysiology [3].
Medical history and clinical examination
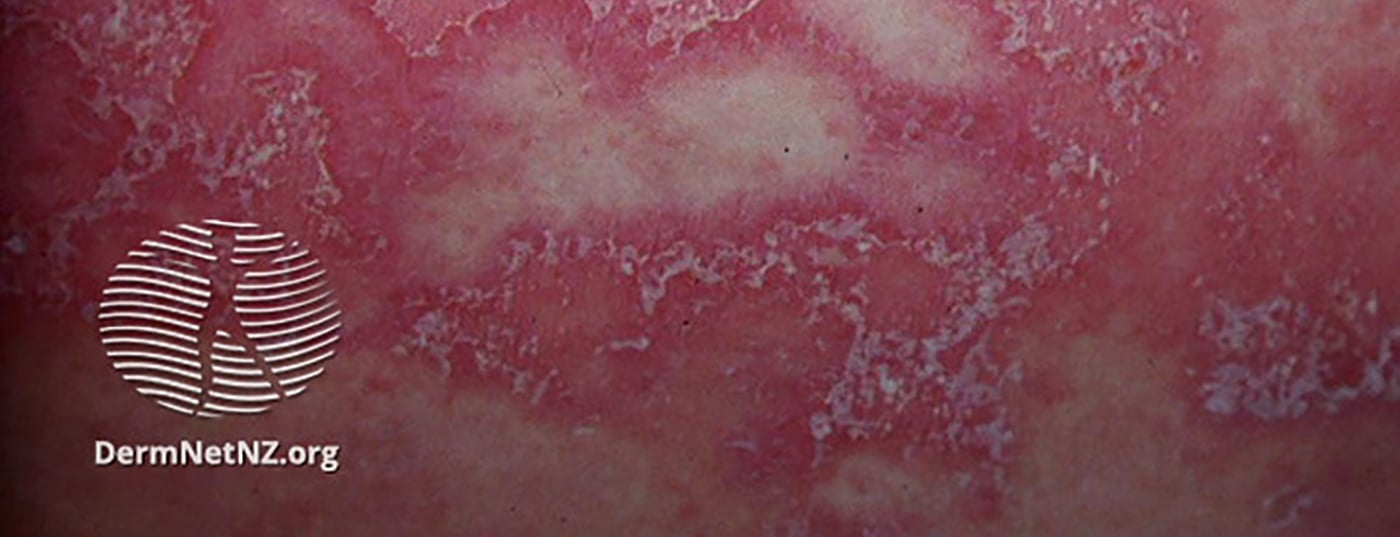
The present case report deals with the case of a 14-year-old girl who had been suffering from pruritic skin lesions on her upper and lower extremities, thighs, and pubic area for two months at initial presentation [4]. Physical examination revealed well-demarcated annular brownish plaques (5-7 cm in diameter) with scaly and raised margins. Multiple pustules were noted, localized over the upper and lower extremities, thighs, and pubic area
Diagnosis and therapy
Initially, tinea corporis was diagnosed. For treatment, terbinafine 250 mg (tbl) plus miconazole cream, twice daily, for two weeks was prescribed [4]. However, the lesions in the lower extremities and on the inner thighs worsened despite treatment compliance. Subsequent histopathologic examination revealed that subcorneal pustules containing neutrophilic leukocytes were located directly beneath the stratum corneum . In addition, there was spongiosis in the epidermis (Fig. 1) [4]. The PAS reaction (“periodic acid-Schiff reaction”) regarding fungal infection was negative. Blood count, blood cell sedimentation rate (ESR), and glucose-6-phosphate dehydrogenase activity and liver function test yielded unremarkable results.

Considering these histopathologic findings in combination with the clinical features, the diagnosis of Sneddon-Wilkinson syndrome/subcorneal pustular dermatosis was reached. Subsequently, drug treatment with dapsone 50 mg daily for two weeks was started, after which the dose was increased to 100 mg daily. The patient showed a good response to therapy.
Discussion
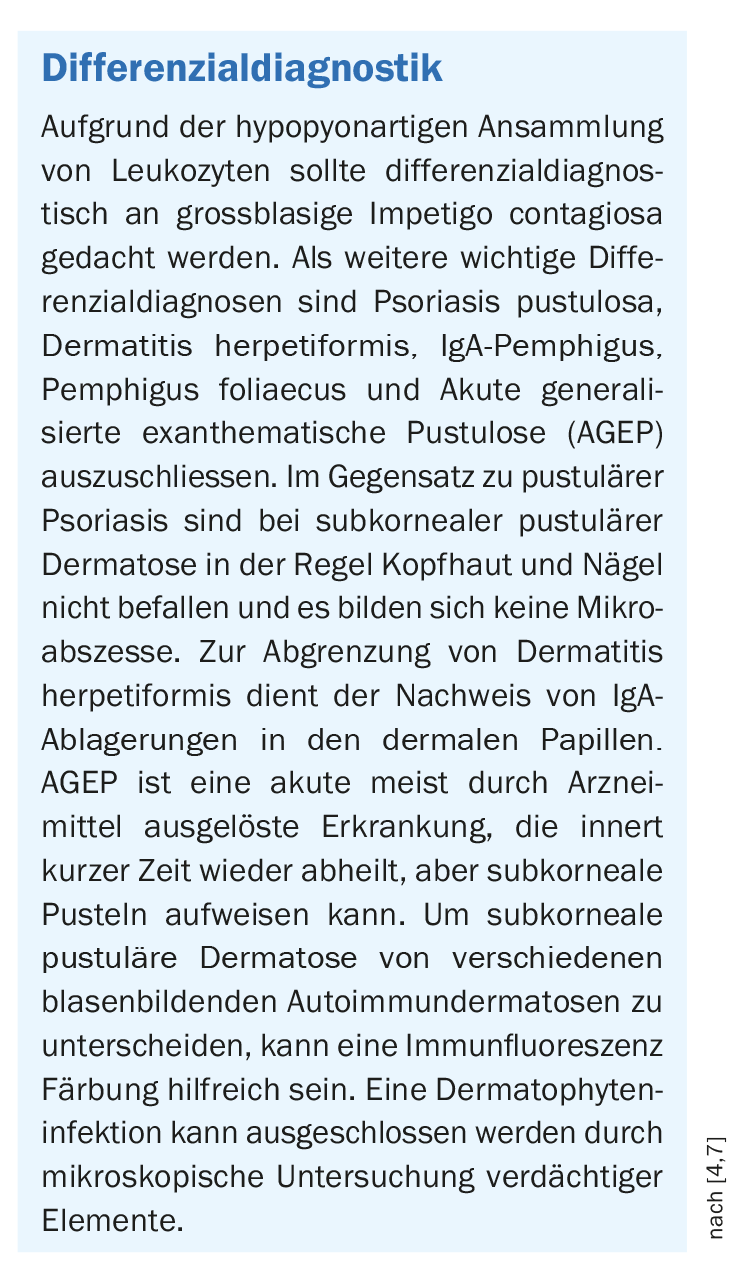
A characteristic feature of subcorneal pustular dermatosis is isolated or grouped flaccid pustules several millimeters in diameter [5]. Histopathologically, unicompartmental subcorneal pustules containing masses of neutrophilic leukocytes are characteristic. The underlying epidermis may have minor acanthotic widening and spongiosis. Subcorneal pustular dermatosis is associated with various systemic diseases such as immunoglobinopathies and lymphoproliferative disorders (e.g., multiple myeloma IgA) [4]. However, in the present case, the patient did not have any systemic diseases. Curative treatment options are currently not available. In the present case, a good response was achieved with dapsone – an active ingredient from the sulfones group with antimicrobial and anti-inflammatory properties [4]. Other treatment options include acitretin, psoralen/PUVA, narrow-band UVB light therapy, colchicine, etretinate, ciclosporin, prednisone, and infliximab [4]. Potent topical corticosteroids can be used as monotherapy or combined with dapsone [6].
Literature:
- Sneddon IB, Wilkinson DS: Br J Dermatol 1956; 68: 385-394.
- Naik HB, Cowen EW: Dermatol Clin 2013, 31: 405-425.
- Watts PJ, Khachemoune A: Am J Clin Dermatol 2016; 17: 653-671.
- Alhafi MA, Janahi MI, Almossalli ZN: Subcorneal Pustular Dermatosis in Paediatrics: A Case Report and Review of the Literature. Cureus 13(12): e20221. doi:10.7759/cureus.20221, Creative Commons Attribution License CC-BY 4.0
- Reed J, Wilkinson J: Subcorneal pustular dermatosis. Clin Dermatol 2000; 18: 301-313. 10.1016/S0738-081X(99)00121-2
- Walkden VM, et al: EJD Eur J Dermatol 1994; 4: 44-46.
- Brown-Falco O, et al. (Eds.): Dermatology and Venereology, 5th edition, Springer: 2005.
DERMATOLOGIE PRAXIS 2022; 32(1): 29