ADHD is a neurodevelopmental disorder that begins in childhood or early adolescence and often persists into adulthood with different trajectories across the lifespan. However, due to a change in symptoms, the disease is often not detected in adulthood. As a result, there is still a clear gap in the treatment of adult ADHD.
Although attention deficit/hyperactivity disorder (ADHD) was first described in 1775 and can therefore look back on a long history, there are still divergent opinions on this disorder, not only among the general public, but also among some experts. In a survey, just half of those questioned stated that they considered the symptoms to be a mental illness. One in five people do not believe that ADHD is a real disorder and most were convinced that childhood ADHD is due to the family-social context. The causes of ADHD are subject to a multifunctional process and are very diverse. One neurobiological cause of the disease is thought to be faulty impulse processing between cortical and subcortical structures in the brain. Pathophysiologically, it is assumed that there is a disturbance in neurotransmitter metabolism, particularly in dopamine and noradrenaline. The hereditary component should not be ignored either.
Symptoms in childhood
The first signs of ADHD can already be detected in infancy. The main characteristics are long crying phases, eating and sleeping problems, refusal of physical contact and restlessness. Of course, all of this can also be observed for a number of other causes, so they are not diagnostic. However, we know from the experience of crying outpatients that infants with early childhood regulatory disorders such as sleep and feeding disorders, dysphoric restlessness, excessive crying, defiance and clinging as well as sleep-wake regulation disorders are more likely to develop ADHD later on. In toddlers, rapid changes in activity, little stamina when playing, conspicuous defiant behavior and an accumulation of accidents or accident-prone behavior stand out. This also applies to motor deficits that become apparent around the second or third year of life. At school age, the typical symptom triad of hyperactivity, inattention and impulsivity is often recognized. Around 3-5% of all children and adolescents are affected by ADHD – boys significantly more often than girls. This makes ADHD one of the most common child psychiatric disorders.
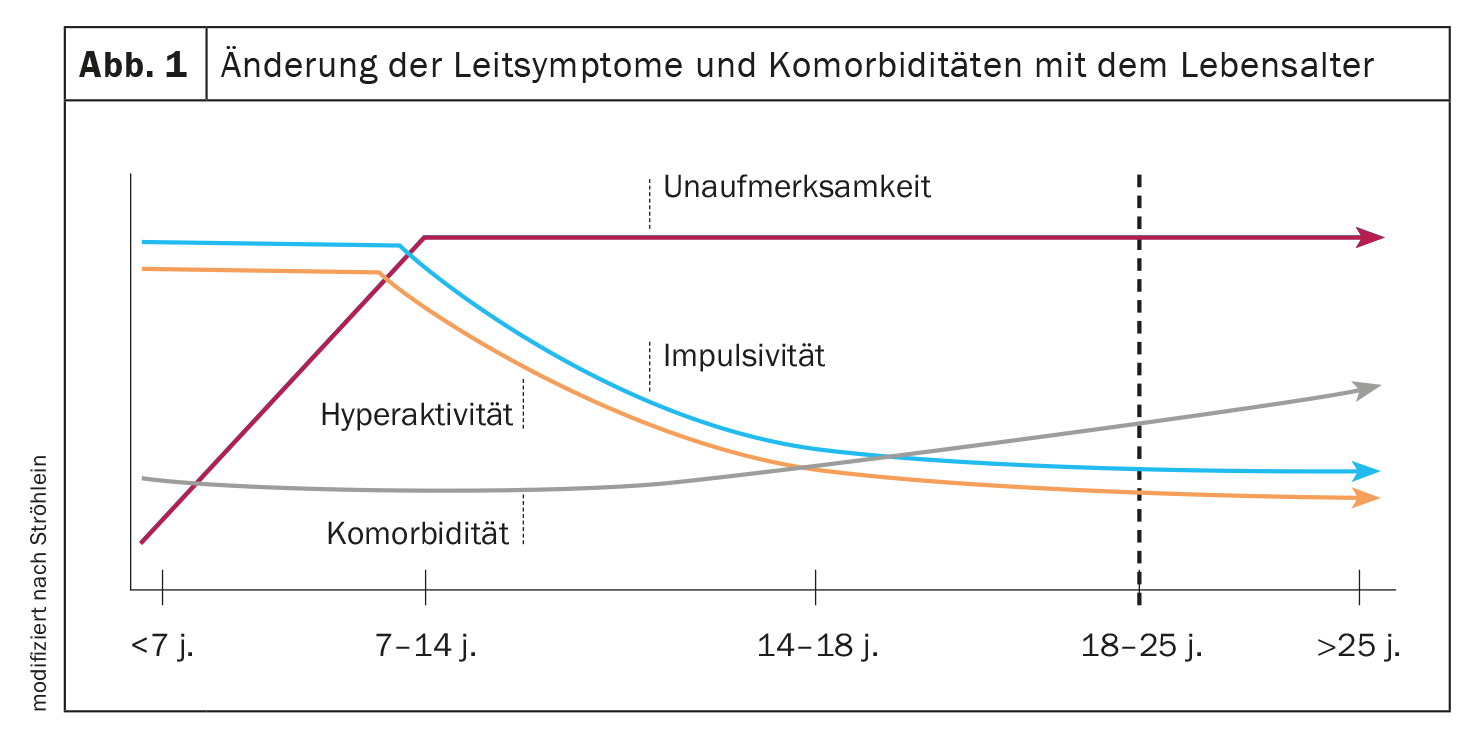
Symptom change in adulthood
ADHD is a chronic disorder with a high tendency to persist. According to estimates by a German group of experts, in up to 80% of cases of ADHD, some or all of the symptoms of the disorder persist in adulthood. However, the typical symptoms can change, so that the disease is perceived differently in adults. The hyperactivity is often no longer acted out, but rather gives way to an inner restlessness. Sitting still for long periods is generally avoided. If this is not possible, many sufferers try to reduce their restlessness by tapping their foot or drumming their fingers continuously. The inattention remains in most cases and is now noticeable in the form of concentration difficulties. Patients remain easily distracted and often have difficulty concentrating on details or distinguishing the important from the unimportant. Impulsivity is also still found in adult ADHD.
When diagnosing ADHD, a distinction is therefore made between subtypes of the disorder, which are dependent on the primary symptoms:
- the ADHD subtype with predominant attention deficit disorder
- the ADHD subtype with predominant hyperactivity and impulsivity
- the ADHD mixed type (with attention deficit disorder plus hyperactivity-impulsivity).
Symptom supplements are a burden for those affected
However, in addition to the main symptoms, many adult ADHD patients also report other symptoms that can significantly restrict their quality of life. These include rash actions, emotional lability, increased irritability, emotional hyper-reactivity and disorganized behaviour. In a doctor’s office, adult ADHD patients stand out, for example, because they repeatedly forget their appointments, fail to bring required documents and often throw the entire office routine into chaos. In addition, ADHD rarely comes alone. It is not uncommon for undiagnosed sufferers to present with depression or an anxiety disorder, for example, which can occur comorbidly with ADHD. The motto here is: Be vigilant!
Further reading:
- Speerforck, et al: JAD 2019; 25: 783-793.
- Purper-Quakil D: Med Sci (Paris). 2010; 26(5): 487-496.
- S3 guideline “Attention deficit/hyperactivity disorder (ADHD) in children, adolescents and adults” (2018), AWMF register number 028-045.
- www.adhs-infoportal.de/adhs-bei-erwachsenen
- Ströhlein B, et al: Transition in ADHD: Critical developmental tasks and their management. NeuroTransmitter 2016; 27.
InFo NEUROLOGY & PSYCHIATRY 2024; 22(3): 30