Hypertension is a widespread disease that primarily affects people of advanced age. Reducing levels to the target range requires comprehensive treatment management consisting of lifestyle modification and pharmacotherapy. If this approach does not lead to the desired success, recent study results show that interventional treatment can also be performed safely.
High blood pressure is a widespread disease, affecting around 18% of the population in Switzerland. The risk of hypertension increases with age. Therefore, Prof. Dr. med. Joachim Weil, Lübeck (D), pursued the question of what influence the environment as well as lifestyle changes can have on the disease. In addition to the environment, genetic and social determinants play a major role in the development of hypertension. Regarding the environment, air pollution is actually a common cause of premature death – five million people die prematurely worldwide due to increased particle pollution. Inhalation of polluted particles leads to oxidative stress, which has effects on the body in the form of autoimmune imbalance or endothelial dysfunction, among others. Systemic inflammation and thromboembolic events can also be attributed to air pollution. The result is cardiovascular events, the expert said. But it also increases the risk of hypertension by about 10%, data show.
Lowering blood pressure levels through lifestyle changes is the first step in the right direction. Appropriate measures include restrictive salt consumption, implementation of a DASH diet, weight reduction, exercise, and abstaining from alcohol consumption. According to studies, improved blood pressure values can certainly be achieved in this way – but as a rule, drug interventions are still necessary to reach the desired target range, summarized the expert.
Individualized therapy management
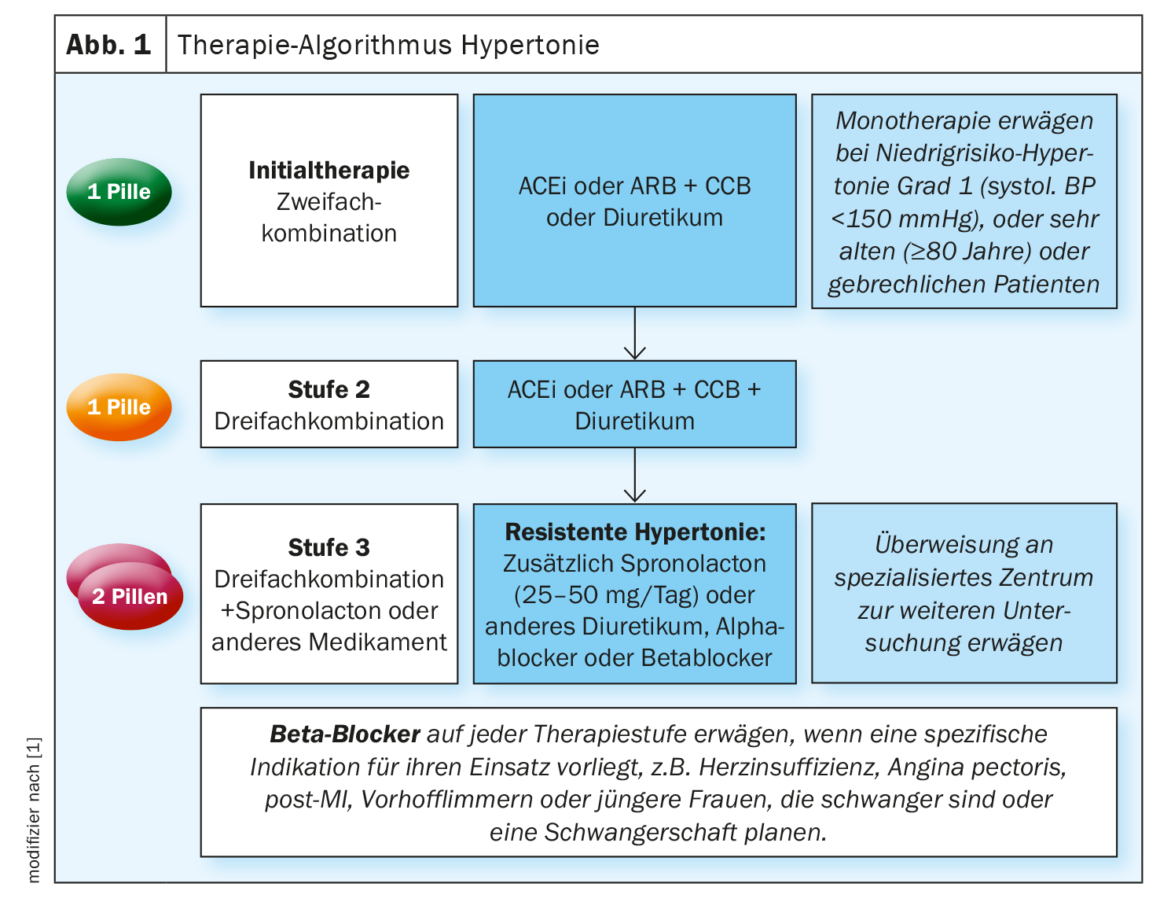
In addition to lifestyle modification, drug treatment should be individualized and take into account age, overall cardiovascular risk, comorbidities, and tolerability of therapy. Recommended initial treatment goal is to lower blood pressure to <140/90 mmHg in all patients. If drug management is well tolerated, values of 130/80 mmHG or lower should then be aimed for, as Prof. Oliver Dörr, MD, Giessen (D), pointed out. In elderly patients 65 years and older, SBP should be in the range of 130-139 mmHg. The guidelines recommend the dual combination of ACEi or ARB in combination with CCB or diuretic as initial therapy (Fig. 1) . The combination should be administered as a single pill, as this has been shown to increase adherence, Dörr emphasized. Monotherapy is indicated only in very old, frail sufferers over 80 years of age and low-risk patients with grade 1 hypotension. Therapy escalation to a triple combination should also be administered in a fixed combination. This consists of an ACEi or ARB plus CCB and diuretic. Resistant hypertension requires referral to a specialized center for further evaluation. As a rule, spironolactone is then added to the triple combination. Beta-blockers can be combined at any therapeutic level if there is a specific indication for their use.
Focus on interventional treatment
In addition to lifestyle modification and individualized pharmacotherapy, modern antihypertensive therapy includes a third pillar – interventional treatment. As Prof. Dr. med. Felix Mahfoud, Homburg (D), explained, some study results regarding device-based treatment have been published recently. No increased safety risk was detected in a total of 1174 patients. A recent ESC Consensus Statement therefore concludes that renal denervation should be considered for adult hypertensives with uncontrolled, resistant disease when long-term drug therapy is not tolerated. However, the general CV risk should be elicited in advance.
Source: “Thinking systemically and treating individually in hypertension,” April 24, 2023, 10:45-12:00, DGIM 2023.
Literature:
- Williams B, et al.: J Hypertens 2018; 36: 1953–2041.
HAUSARZT PRAXIS 2023; 18(6): 45