Since their introduction in the 1990s, bisphosphonates have been the drugs of first choice in the treatment of osteoporosis. They inhibit osteoclast-mediated resorption and bone remodeling, increase bone mineral density, and reduce the risk of hip and vertebral fractures by 40 to 70%. Nevertheless, their reputation has suffered – whether justifiably, US researchers wanted to find out.
Case reports of unusual fragility fractures in the subtrochanteric region and along the femoral diaphysis in patients treated with bisphosphonates became known in the mid-2000s, and were followed by larger studies of these fractures (now termed atypical femur fractures) and their relationship to bisphosphonates. These reports and studies have led to a significant decline in bisphosphonate use despite its proven efficacy and favorable benefit-risk profile, write Professor Dennis M. Black, M.D., of the Department of Epidemiology and Biostatistics at the University of California, and colleagues [1]. However, according to them, considerable ambiguity remains regarding the extent of the association between bisphosphonates and atypical fractures: some studies had shown a minimal risk, while others showed a clear association, especially with prolonged use.
To get to the bottom of this, researchers analyzed patient data from a Southern California health insurance company in a prospective cohort study. Their hypothesis: the risk of atypical fracture is related to the duration of bisphosphonate use but attenuates after adjustment for several clinical variables.
Women aged 50 years and older who had received at least one prescription for oral or i.v. bisphosphonate for osteoporosis were included. The primary outcome was the occurrence of atypical femur fracture, and the observation period was 10 years. Potential cases of atypical fractures were selected using the International Classification of Diseases (ICD) diagnosis codes for subtrochanteric femoral shaft fractures.
Absolute risk of atypical femur fracture remained low
Among the 196 129 women, 277 atypical femur fractures occurred and 9102 hip fractures. Women aged 65 to 84 years had higher atypical fracture rates than younger women or those older than 85, but the incidence of hip fracture increased with age. With increasing duration of bisphosphonate use, the incidence of atypical fractures in women with less than 3 months of use increased from 0.07 per 10 000 person-years to 13.10 in women with 8 years or more. When the bisphosphonate was discontinued, the rate of atypical fractures decreased over time (Fig. 1) . The result reflects differences in ethnicity. Smaller body size and higher body weight or additional glucocorticoid therapy also provided an increased risk of atypical fractures.
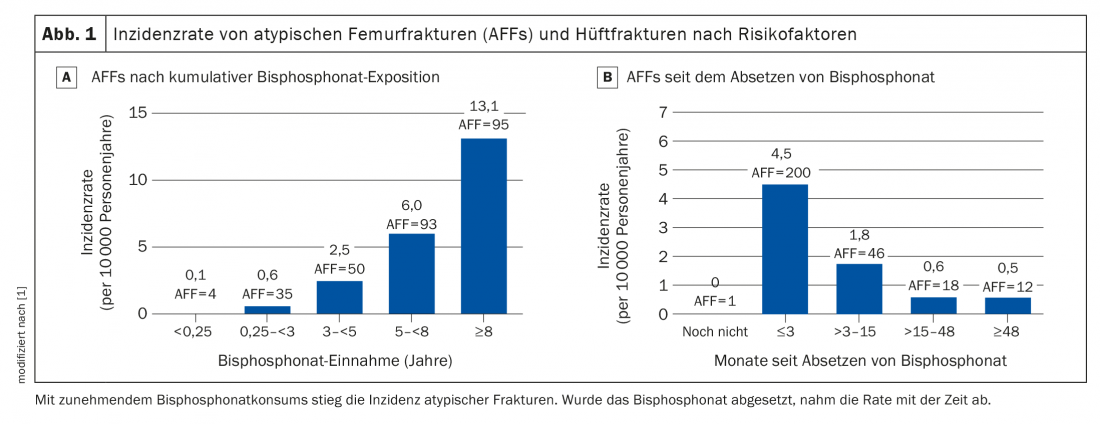
In Caucasian women, the number of fractures prevented for each fracture type at all time points far outweighed the atypical fractures associated with bisphosphonate. Thus, after 3 years, 149 hip fractures were prevented by treatment with bisphosphonates, with only 2 atypical fractures associated with this class of agents. A similar picture emerged in women of Asian ethnicity, although the ratio was somewhat less favorable, with 91 osteoporosis-related or hip fractures with 8 atypical fractures associated with medication.
The findings support previous studies showing that the absolute risk of atypical femur fracture is very low compared with the greater number of fractures effectively prevented by bisphosphonates, Prof. Black and colleagues write. That the oldest women, who are at highest risk for hip and other fractures, had the lowest risk for atypical fractures is a risk relationship that could be used in the future to individualize clinical decisions about bisphosphonate therapy and better calculate related risk, he said. The difference between ethnic groups also affects the risk-benefit ratio of bisphosphonate treatment and could influence decisions regarding treatment initiation and duration. However, the researchers caveat that their risk-benefit comparison is based only on the number of fractures. A more complete comparison would also consider costs plus associated morbidity and mortality.
Literature:
- Black DM, et al: N Engl J Med 2020; 383: 743-753; doi: 10.1056/NEJMoa1916525.
HAUSARZT PRAXIS 2020; 15(12): 47