Delirium, an acute confused state, was the focus of a presentation at the ESCIM Congress in Geneva. Some of the key points discussed revolved around the proper definition of this condition, the predisposing and precipitating factors, and possible management approaches. As an expert, Prof. Gabriel Gold, MD, of Geneva University Hospitals, presented a broad overview of the topic.
(ag) First, Prof. Gabriel Gold, MD, University Hospitals of Geneva, answered the question of how to define delirium in the first place: “According to DSM V, it is an acute confused status with altered consciousness and attention that ends in a cognitive disorder that cannot be better described by a preexisting condition. Delirium fluctuates in severity and appears to be due to a presenting medical condition.” The prevalence in the general population is 1- 2%, with delirium being particularly common during hospitalization in the intensive care unit and in patients with dementia.
Predisposing factors are summarized in Table 1.

Triggering factors may include: psychoactive drugs, physical restraints, urinary catheter, elevated serum urea levels, electrolytic disturbance, infections, and iatrogenic events [1]. Further research concludes that polypharmacy, the presence of various medical conditions, malignancy, or even surgery, as well as pain and abnormal serum albumin levels, may also result in delirium.
“Consequently, delirium is usually multifactorial, which is why targeting a single risk factor can hardly be efficient. Rather, broad approaches are useful to prevent or resolve delirium,” the expert said.
Significantly worse prognosis
Not only does delirium increase mortality, e.g., in the intensive care unit or emergency department, but also the risk of cognitive decline or institutionalization.
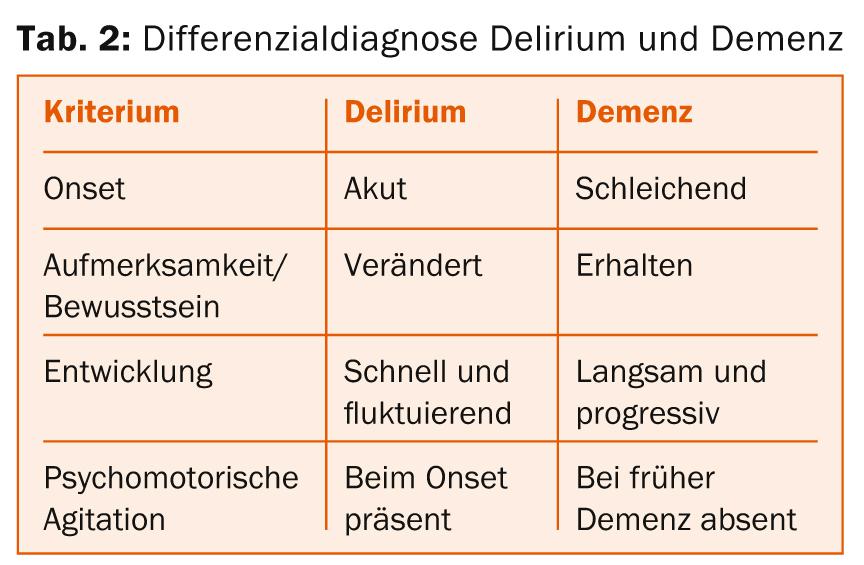
“Cognitive impairment must be differentiated into delirium, dementia, and depression for differential diagnosis,” Prof. Gold explained (Table 2).
“More than 20 different diagnostic tools exist to detect delirium, yet delirium is often misdiagnosed or underdiagnosed. The most widely used is the so-called Confusion Assessment Method (CAM) [2]. The sensitivity is 94, and the specificity is 89%. There are adapted versions for use in the ICU. Thus, it is by far the best diagnostic tool currently available.” Four points are critical in CAM [2]:
- The acute onset and fluctuating course (reliable history with the help of caregivers and family members to document acute changes in mental status and fluctuations throughout the day).
- Inattention (difficulty focusing attention; easily distracted).
- Disorganized thinking (incoherent, rambling, irrelevant conversation; illogical flow of thought; unpredictable topic jumps)
- Altered consciousness (alert, hyperalert; lethargic but easily aroused; stuporous and not easily aroused; comatose and not aroused at all).
The diagnosis of delirium requires the presence of items 1 and 2 and one or both of items 3 and 4.
Management
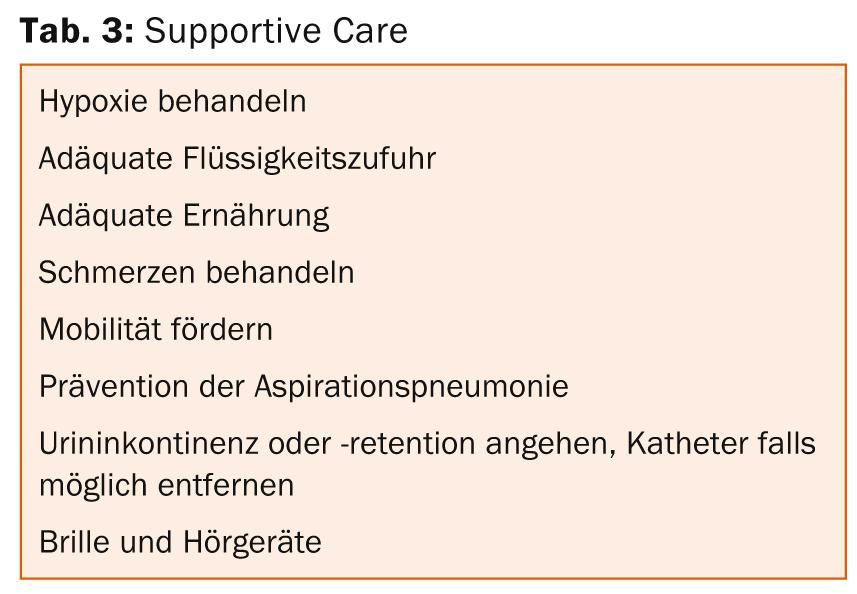
In addition to specific treatment of the underlying disease and general support measures, as shown in Table 3 , behavioral management is also critical.
“Whenever possible, physical restraint should be avoided and the presence of familiar people and things should be encouraged. Neuroleptics that can be considered are haloperidol in low doses and possibly atypical neuroleptics such as quetiapine, ripseridone, or olanzapine [3]. Benzodiazepines and cholinesterase inhibitors such as rivastigmine should not be used, as these have no effect in prevention and only increase the number of side effects. The preventive effect of neuroleptics has also been studied. The results are inconsistent so far,” Prof. Gold concluded.
Source: “How to deal with delirium,” seminar at ESCIM Congress, May 14-16, 2014, Geneva.
Literature:
- Inouye SK, Westendorp RG, Saczynski JS: Delirium in elderly people. Lancet 2014 Mar 8; 383(9920): 911-922.
- Inouye SK, et al: Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990 Dec 15; 113(12): 941-948.
- Yoon HJ, et al: Efficacy and safety of haloperidol versus atypical antipsychotic medications in the treatment of delirium. BMC Psychiatry 2013 Sep 30; 13: 240.
InFo NEUROLOGY & PSYCHIATRY 2014, 12(4): 36-37.











