Firstly, lifestyle measures, secondly metformin, thirdly individualization – according to Prof. Marc Donath, MD, Basel, Switzerland, this is how type 2 diabetics are treated today. Depending on the individual situation, either DPP4 inhibitors, GLP-1 analogues or basal insulin are used in the third step.
Lifestyle measures, when applied consistently and over the long term, can make a very large contribution to the control of diabetes and are therefore at the forefront of every type 2 diabetic’s treatment. “Give your patients concrete instructions for incorporating physical activity into their daily routine and emphasize the positive effects of this measure. When it comes to diet, you should not use prohibitions either, but rather encourage patients to really enjoy eating again,” advised Prof. Marc Donath, MD, Basel, to the audience at a satellite symposium at the SGIM Congress in Basel. If these measures are not sufficient, drug therapy with metformin is started. “Metformin is still the best drug prognostically, and you should really never stop it,” Prof. Donath emphasized. Lactic acidosis is really only a problem in patients with renal insufficiency. Swiss diabetologists have agreed that metformin should be given safely up to a GFR of 45 ml/min and safely not given above a GFR ≤30 ml/min. For values in between, it is at the discretion of the treating physician whether or not to give metformin in the individual case.
Individualize therapy
Only in a third step, if the target blood glucose levels are not reached despite lifestyle measures and metformin, does the individualized expansion of treatment follow (Tab. 1) . Prof. Donath recommends adding a DPP4 inhibitor in the first instance. Compared with sulfonylureas, gliptins have the advantage of being weight neutral and, most importantly, do not cause hypoglycemia.
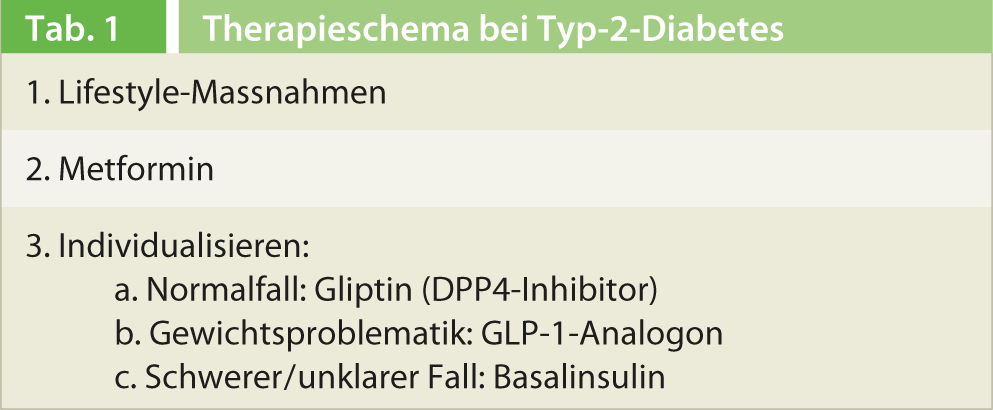
Overall, there are no major differences between the various DPP4 inhibitors; from case to case, one or the other preparation is more suitable. If the weight problem is in the foreground, Prof. Donath advises the administration of a GLP-1 analog. A distinction must be made here between short-acting preparations administered prandially, which delay gastric emptying and thus have a pronounced effect on postprandial blood glucose, and long-acting preparations administered once daily or even only once a week, which act mainly on fasting blood glucose.
In severe type 2 diabetics and in unclear cases, basal insulin is ideally given. “Insulin is always right in principle. It is never wrong to give insulin because all diabetics, including type 2 diabetics, have an insulin deficiency,” Prof. Donath explained. The so-called treat-to-target regimen has proven effective here, in which one starts with 10 IU of a basic insulin and gradually increases the dose until the target blood glucose value is reached. After three months, HbA1c is measured; if the target value has not yet been reached, an oral antidiabetic (primarily a DPP4 inhibitor) or a GLP-1 analogue is also given.
Source: “Type 2 diabetes – The right therapy for the right patient”. Satellite Symposium of Bristol-Myers Squibb and AstraZeneca at the SGIM Congress, May 29-31, 2013, Basel.