Acclimatization to increasing altitude results in various physiological adaptations. When are these non-pathological vs. pathological phenomena? What is known about prevention and treatment of altitude sickness in children and adolescents?
Family vacations in high altitude areas such as the Himalayas and Andes are seeing an increase in popularity. However, a Swiss family does not have to travel far to be exposed to altitude, as families already travel to altitudes above 2000 m for hiking and skiing vacations in Switzerland. This also increases the number of visits to the doctor to prepare for the altitude and provide information on the prevention of altitude sickness, especially for children. We would like to give you a backpack to be prepared for this.
What happens at high altitude?
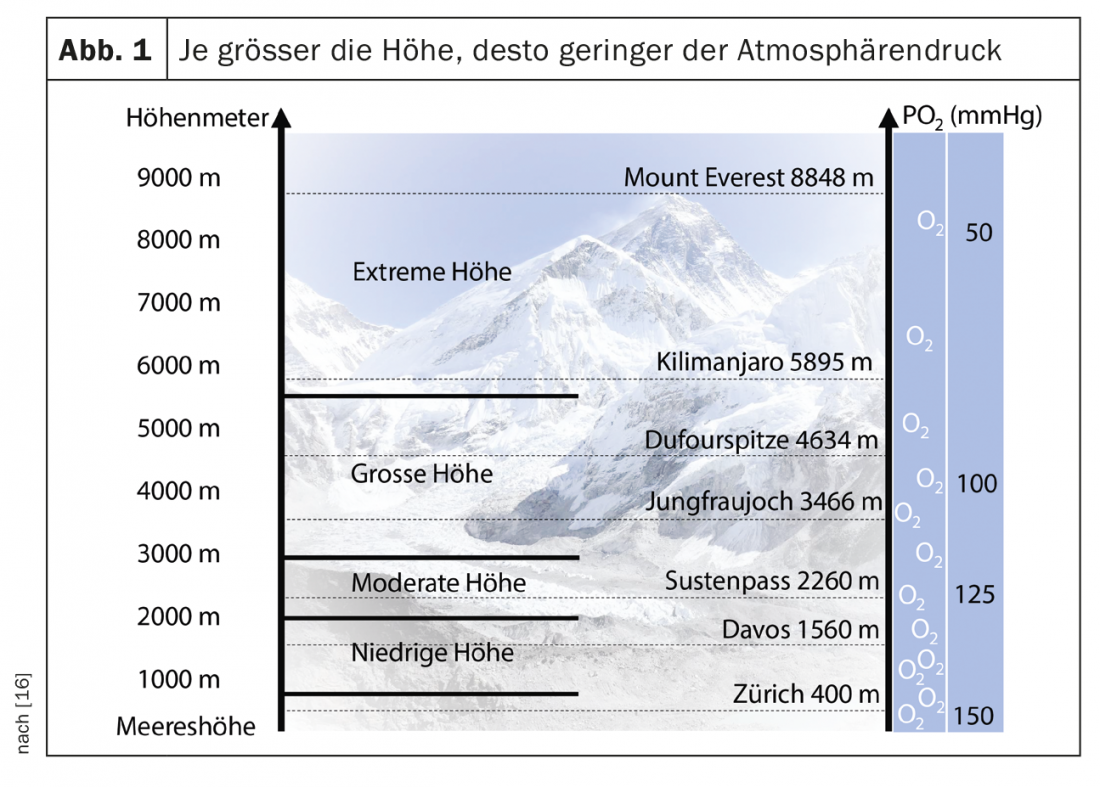
The air we breathe every day contains 21% oxygen. At sea level, a large pressure differential exists for oxygen, which allows oxygen to easily enter the tissues. If we leave the lower altitudes and go to high altitudes, the air still contains 21% oxygen, but the atmospheric pressure continuously decreases so that the tissue in the periphery becomes hypoxic (Fig. 1). Chemoreceptors in the periphery react to this and cause our body to breathe more (hyperventilation). The heart rate increases. These processes become more apparent the higher you climb. Both mechanisms contribute to an increase in blood oxygen saturation and are referred to as acute adaptation. If one spends several days and weeks at altitude, the body responds with further subacute and chronic adaptations. These include a further increase in respiration, a reduction in blood plasma volume, bicarbonate excretion by the kidneys (to neutralize respiratory alkalosis), and especially increased red blood cell production. These are all important chronic adaptations that lead to further increases in oxygen-carrying capacity [1]. Although there are no data on acclimation in children, it is likely that these mechanisms apply equally to children.
If this acclimatization does not happen without problems, the body suffers. There are three main types of altitude sickness: acute mountain sickness (AMS), high altitude pulmonary edema (HAPE), and high altitude cerebral edema (HACE). ABK develops already at lower altitudes from 2500 m and can be treated well, while HAPE and HACE occur mainly at altitudes from 4000 m and are life-threatening diseases.
The most common evil: acute mountain sickness
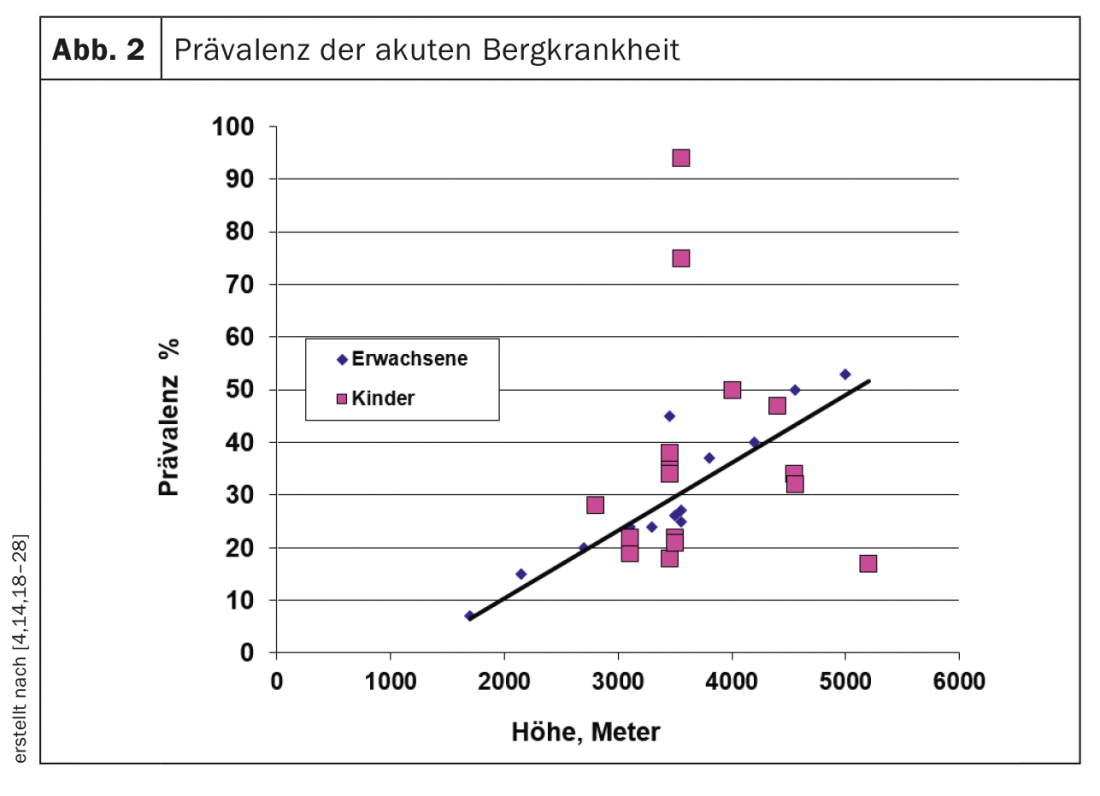
Acute mountain sickness (ABK) is the most common altitude sickness. It increases with increasing altitude regardless of age (fig. 2). The prevalence in children is comparable to that in adults, although the variability in the different studies is greater than in adults, probably due to the small numbers of cases, different diagnostics and rates of ascent. In a representative study conducted at Jungfraujoch (3450 m), the prevalence was 30% in children, 37% in adolescents, and 45% in adults [2].
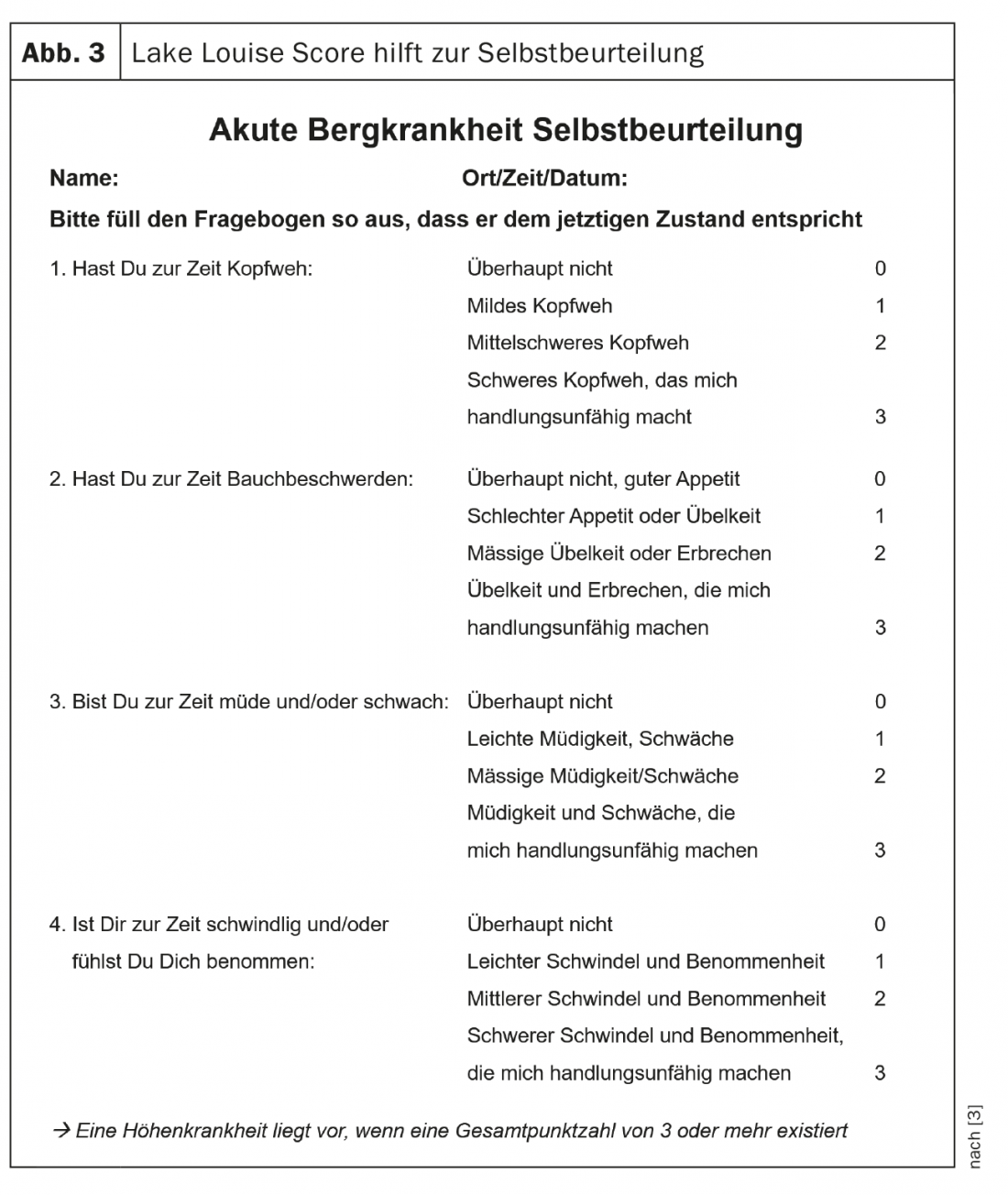
Diagnostic criteria for ABK are acute exposure to altitude (>2500 m) and the presence of specific symptoms, which usually appear only after a stay of 4-12 hours. The cardinal symptom of ABK is headache, often accompanied by nausea, fatigue, dizziness and sleep disturbances. To diagnose ABK, a score is calculated from the four main symptoms (headache, nausea/vomiting, fatigue, and dizziness). A score of at least 3 is required for the diagnosis of ABK (Lake Louise scoring system). Controversy exists as to whether headache must be a compelling part of the diagnosis, as defined in the most recent adult guidelines [3]. Our experience shows that children in particular do not always complain of headache, although all other symptoms are present [2].
There is an increased risk of experiencing an ABK with rapid rise, increasing altitude, and age less than six years. Individual studies, but not all [4], suggest a genetic predisposition [2].
The Lake Louise scoring system [3] is a simple tool to diagnose ABK and determine its severity (Fig. 3). It can also be used in children from 8-9 years of age. Care should be taken with younger children, as they often cannot complain in a symptom-specific manner. For this reason, it is also not advisable to rely on the LakeLouise scoring system for young children, even though it was developed specifically for this age [5]. The most important basic rule for younger children is: if the child’s behavior is not normal (regarding playing, eating, sleeping, interaction with other children and adults), it must be assumed that the child has ABK and must be dismounted.
Dangerous high altitude pulmonary edema
High altitude pulmonary edema (HAPE) is a non-cardiac induced pulmonary edema caused by hypoxia. Cardinal symptom is reduced exercise capacity combined with pulmonary symptoms such as dyspnea at rest and cough on exertion. This is followed by dyspnea at rest, rales, cyanosis, cough at rest, and partial appearance of pink discolored frothy sputum [6]. Although a HAPE from 3000 m, it usually manifests itself from an altitude of 4000 m. The prevalence ranges from 0.2-15%, depending on the altitude reached and the rate of ascent: 0.2% for an ascent to 4500 m within four days, 15% with an ascent to 5500 m in one to two days. The risk of HAPE is significantly increased in mountaineers who have had a history of HAPE – impressively up to 60%. HAPE is a life-threatening disease. If left untreated, 50% of affected adults die. Data for children are missing so far.
HAPE is triggered by an exuberant response of pulmonary artery pressure to hypoxia, in that both arterial and capillary pressures become so great that fluid leaks into the interstitium and alveoli through a so-called capillary leak and secondary inflammatory processes. Children living in the lowlands are likely to have the same risk as adults of developing HAPE. Again, a genetic predisposition with clustering within families is suspected [7,8].
However, children living at ≥3000 m appear to be at higher risk of developing what is termed “re-entry HAPE” [9]. These children develop a HAPE after returning to high altitude after only two days in the lowlands. This appears to be more common in children than adults. This occurrence must be taken into account when families live at higher altitudes in the long term. More important for our latitudes is the fact that respiratory infections just before or during altitude exposure favor the risk of developing HAPE in children, this probably through the release of inflammatory mediators [10]. Children with cardiac vitiation are especially at risk.
Rapidly fatal: high-altitude cerebral edema
High altitude cerebral edema (HACE) is a life-threatening vasogenic cerebral edema triggered by hypoxia and manifested by altered consciousness and ataxia. Cerebral pressure symptoms with pain therapy-resistant headache and vomiting are typical, although headache in particular may be masked by the altered state of consciousness. HACE occurs practically only at altitudes above 4000 m with a prevalence of 0.5-1%, where it usually appears after two days. It is extremely rare in children, so our knowledge is limited to only a few case reports [11]. Nevertheless, HACE can occur during treks to remote areas, which are nowadays also undertaken by families with children. If it is not recognized quickly and treated immediately, or if immediate relevant descent is not possible, the lethality is extremely high.
Special populations
Newborns and toddlers: Time and again, parents ask whether they can travel at altitude with children in their first year of life. Currently, no convincing data exist to support an increased risk of sudden infant death syndrome at altitude. Prolonged hypoxic states were measured in individual experimental studies, with various methodological deficiencies in one highly ranked publication in particular [12]. Nevertheless, caution is recommended, especially when sleeping unattended at altitudes above 2500 m, as immature breathing may be present especially in the first months of life [13]. Short-term hikes are no problem in any case.
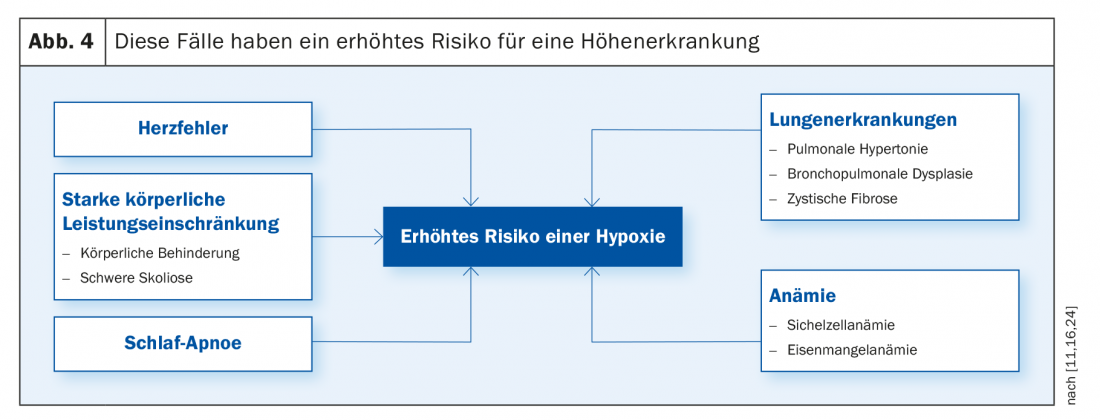
Children at increased risk: In general, children and adolescents with a chronic condition that involves or more rapidly achieves hypoxemic states are at increased risk of developing altitude sickness or complication at altitude (Fig.4). Particular caution should be exercised in children and adolescents with combined risks of increased hypoxemic states – such as Down syndrome (cardiac vitiation, sleep apnea) or cystic fibrosis (lung disease, pulmonary hypertension). Actually, these sick young people do not belong at altitudes above 2000 m. Exceptionally, in the case of mild disease and a symptom-free stress test in the lowlands without desaturation, moderate altitude exposure may be granted.
Prevention of altitude sickness
Table 1 provides recommendations for preventing altitude sickness in children and adults. It is advised not to climb higher than 300-500 m per day and to take a rest day every three days. Pre-acclimatization to altitudes of at least 3000 m with physical activity one to two months prior is ideal, as such may reduce the incidence of ABK in adults [14]. Certainly one reduces the risk of altitude sickness by a one-week acclimatization to altitudes between 2000-3000 m, timed as close as possible before further exposure to altitude [15]. In general, when accompanied by children, one should be very flexible in the ascent plan, guided primarily by the well-being of the children and, of course, the adults.
In general, pharmacological prevention is not recommended in children and adolescents. Slow ascension (defined in Table 1) can usually avoid the need to take medications [16]. Trekking or mountaineering at altitude is a recreational activity. In addition, taking medication can cause side effects. In rare cases, the use is nevertheless necessary, especially when professional or logistical conditions make a slow rise impossible.
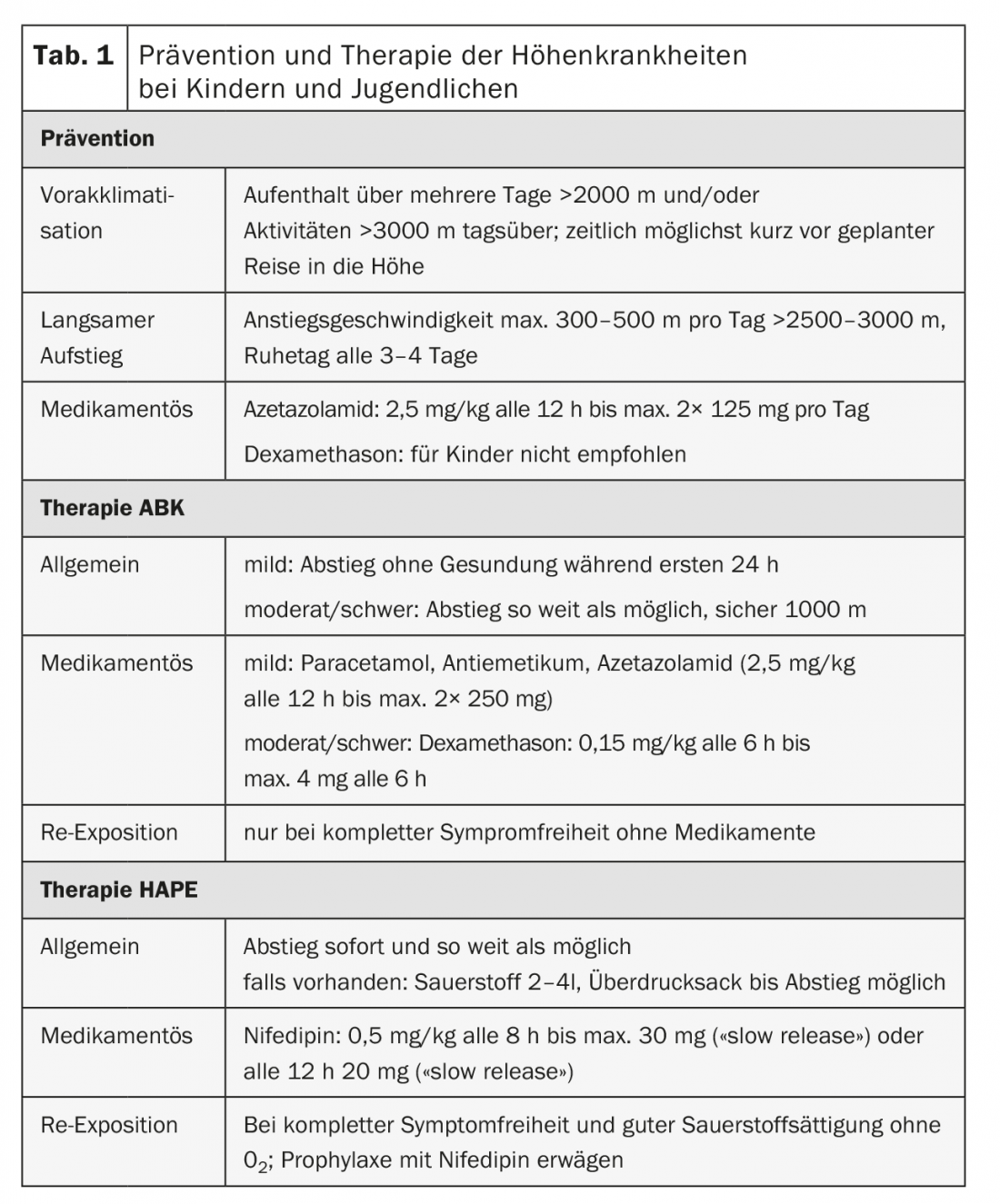
Medication-wise, there is an option to use acetazolamide if there is an increased risk of ABK. In case of intolerance, dexamethasone is considered an alternative. Indication for drug prophylaxis in children and adolescents exists when ABK has existed at a comparable altitude profile or when, in the absence of previous or milder exposure, the ascent is more rapid (>500 m/day above 3000 m or within one day to altitudes >3000 m). Acetazolamide should be started one day prior to exposure. Use is indicated until two days can be spent at a certain altitude without symptoms or until descent is made. Drug side effects are in the form of paresthesias in fingers and toes (35-90% of adults), initial polyuria (8-55% of adults), and unpleasant change in taste when consuming carbonated beverages (4-14% of adults). Because of the risk of relevant side effects when taking dexamethasone (hyperglycemia, suppression of the adrenal cortex, psychological changes), this use should be limited to a few days. In addition, dexamethasone may only be used for very specific indications (documented intolerance of acetazolamide or unavoidable rapid exposure at high altitude).
How to treat?
The therapy of altitude sickness can usually be avoided by the preventive measures described above. If symptoms still occur, a day of rest with symptomatic therapy (acetaminophen for headache, antiemetics) can be arranged if ABK is mild. If symptoms persist for more than 24 hours, descend by 500-1000 m. Therapeutic use of acetazolamide may be attempted in mild ABK, but good studies are lacking. If descent cannot be achieved and pronounced symptoms persist, there are three therapeutic options: Dexamethasone every six hours, supplemental oxygen (2-4 l/min), or the use of a hyperbaric bag that reduces the effective altitude by 2000 m [17]. These therapies have been evaluated in adults. They are recommended by many experts [11,16] also for children, although this is not backed up by studies.
If HAPE or HACE is suspected to be incipient, descent should be made immediately to save life, whenever possible in a passive manner to prevent even more massive exercise-induced hypoxemia, which can be fatal. If this is not possible for logistical or weather reasons, nifedipine can significantly reduce pulmonary arterial pressure and can be ideally used in children with virtually no side effects. In HACE, dexamethasone at the above dosage should be used in addition to descent (again, study data are lacking to date).
The trip to the heights should be an experience for the family and not an ordeal. Often, altitude sickness is not the problem – rather, some families are faced with entirely different problems that could have been prevented with proper travel planning and preparation. The box provides useful tips on how to remedy this.
Take-Home Messages
- The most common is acute mountain sickness (ABK, from 2500 m altitude), the severity of which can be assessed using the Lake Louise scoring system. This focuses on the four main symptoms of headache, nausea/vomiting, fatigue and dizziness.
- High altitude pulmonary edema (HAPE, from 3000 m altitude) is manifested by reduced physical performance, dyspnea and cough.
- High altitude cerebral edema (HACE, from 4000 m altitude) manifests itself by headache, vomiting and changes in consciousness.
- Data on children’s exposure to altitude and its health consequences are scarce.
- If children are traveling to high altitudes, it is recommended to climb as conservatively as possible and to plan flexibly. This minimizes the risk of mountain sickness as well as the use of medication.
- In principle, it is important to be well prepared for altitude. In addition, climb slowly (300-500 m/day from 2500 m). At
- Suspected HAPE or HACE and severe ABK should be descended immediately. Drug therapy with acetazolamide, nifedipine, or dexamethasone should always be considered.
Literature:
- Schommer K, Bartsch P: Basic medical advice for travelers to high altitudes. Dtsch Arztebl Int 2011; 108(49): 839-847.
- Kriemler S, et al: Prevalence of acute mountain sickness at 3500 m within and between families: a prospective cohort study. High Alt Med Biol 2014; 15(1): 28-38.
- Roach RC, et al: The 2018 Lake Louise Acute Mountain Sickness Score. High Alt Med Biol 2018; 19(1): 4-6.
- Rexhaj E, et al: Reproducibility of acute mountain sickness in children and adults: a prospective study. Pediatrics 2011: 127(6): e1445-1448.
- Meijer HJ, Jean D: Children at altitude. Recommendations of the UIAA Medical Commission 2008.
- Bärtsch P, Swenson ER: Acute high-altitude illnesses. N Engl J Med 2013; 369(17): 1666-1667.
- Kriemler S, et al: Higher pulmonary artery pressure in children than in adults upon fast ascent to high altitude. Eur Respir J 2008; 32(3): 664-669.
- MacInnis MJ, Koehle MS, Rupert JL: Evidence for a genetic basis for altitude illness: 2010 update. High Alt Med Biol 2010; 11(4): 349-368.
- Scoggin CH, et al: High-altitude pulmonary edema in the children and young adults of Leadville, Colorado. N Engl J Med 1977; 297: 1269-1272.
- Durmowicz AG, et al: Inflammatory processes may predispose children to high-altitude pulmonary edema. J Pediatr 1997; 130(5): 838-840.
- Pollard AJ, et al: Children at high altitude: an international consensus statement by an ad hoc committee of the International Society for Mountain Medicine, March 12, 2001. High Alt Med Biol 2001; 2(3): 389-403.
- Parkins KJ, et al: Effect of exposure to 15% oxygen on breathing patterns and oxygen saturation in infants: interventional study. BMJ 1998; 316(7135): 887-891.
- Niermeyer S: Cardiopulmonary transition in the high altitude infant. High Alt Med Biol 2003; 4(2): 225-239.
- Schneider M: Acute mountain sickness: influence of susceptibility, preexposure, and ascent rate. Med Sci Sports Exerc 2002; 34(12): 1886-1891.
- Muza SR, Beidleman BA, Fulco CS: Altitude preexposure recommendations for inducing acclimatization. High Alt Med Biol 2010; 11(2): 87-92.
- Garlick V, O’Connor A, Shubkin CD: High-altitude illness in the pediatric population: a review of the literature on prevention and treatment. Curr Opin Pediatr 2017; 29(4): 503-509.
- Bärtsch P, et al: Treatment of acute mountain sickness by simulated descent: a randomised controlled trial. BMJ 1993; 306(6885): 1098-1101.
- Theis MK: Acute mountain sickness in children at 2835 meters. Am J Dis Child 1993; 147: 143-145.
- Pollard AJ, Murdoch DR, Bartsch P: Children in the mountains. BMJ 1998; 316: 874-875.
- Moraga FA, Osorio JD, Vargas ME: Acute mountain sickness in tourists with children at Lake Chungara (4400 m) in northern Chile. Wilderness Environ Med 2002; 13: 31-35.
- Yaron M, et al: Evaluation of diagnostic criteria and incidence of acute mountain sickness in preverbal children. Wilderness Environ Med 2002; 13: 21-26.
- Imray CH, et al: Self-assessment of acute mountain sickness in adolescents: a pilot study. Wilderness Environ Med 2004; 15: 202-206.
- Moraga FA, Pedreros CP, Rodriguez CE: Acute mountain sickness in children and their parents after rapid ascent to 3500 m (Putre, Chile). Wilderness Environ Med 2008; 19: 287-292.
- Yaron M, Niermeyer S: Travel to high altitude with young children: an approach for clinicians. High Alt Med Biol 2008; 9: 265-269.
- Bloch J, et al: Prevalence and time course of acute mountain sickness in older children and adolescents after rapid ascent to 3450 meters. Pediatrics 2009; 123: 1-5.
- Dallimore J, Rowbotham EC: Incidence of acute mountain sickness in adolescents. Wilderness Environ Med 2009; 20: 221-224.
- Pradhan S, et al: Acute mountain sickness in children at 4380 meters in the Himalayas. Wilderness Environ Med 2009; 20: 359-363.
- Stokes SH, et al: Adolescents with altitude: young people do well on Kilimanjaro. Arch Dis Child 2009; 94: 562-563.
HAUSARZT PRAXIS 2019; 14(1): 25-29











