Because ovarian cancer generally has no specific symptoms, it is often diagnosed at late stages. The mortality risk is correspondingly high. In order to provide affected women with optimal therapy, treatment should follow guidelines. In fact, such an approach significantly increases the probability of survival. The S3 guideline has now been updated.
Every year, an average of 580 women in Switzerland develop ovarian cancer, 430 of whom do not survive the disease [2]. 70% of cases are diagnosed only at advanced stages (FIGO IIB-IV) [1,2]. But then the 5-year survival rate is already below 40%. Accordingly, early diagnosis and effective therapy are important. Above all, this should be done in accordance with guidelines. Studies have shown that after three years, 60% of patients treated according to guidelines are still alive, compared with only 25% of those treated suboptimally [1]. Under the auspices of the German Society of Gynecology and Obstetrics (DGGG), the Oncology Guideline Program has updated the S3 guideline “Diagnosis, Therapy and Follow-up of Malignant Ovarian Tumors”. In the sense of a “living guideline”, this is done annually, taking into account current study results.
Prophylaxis rethought
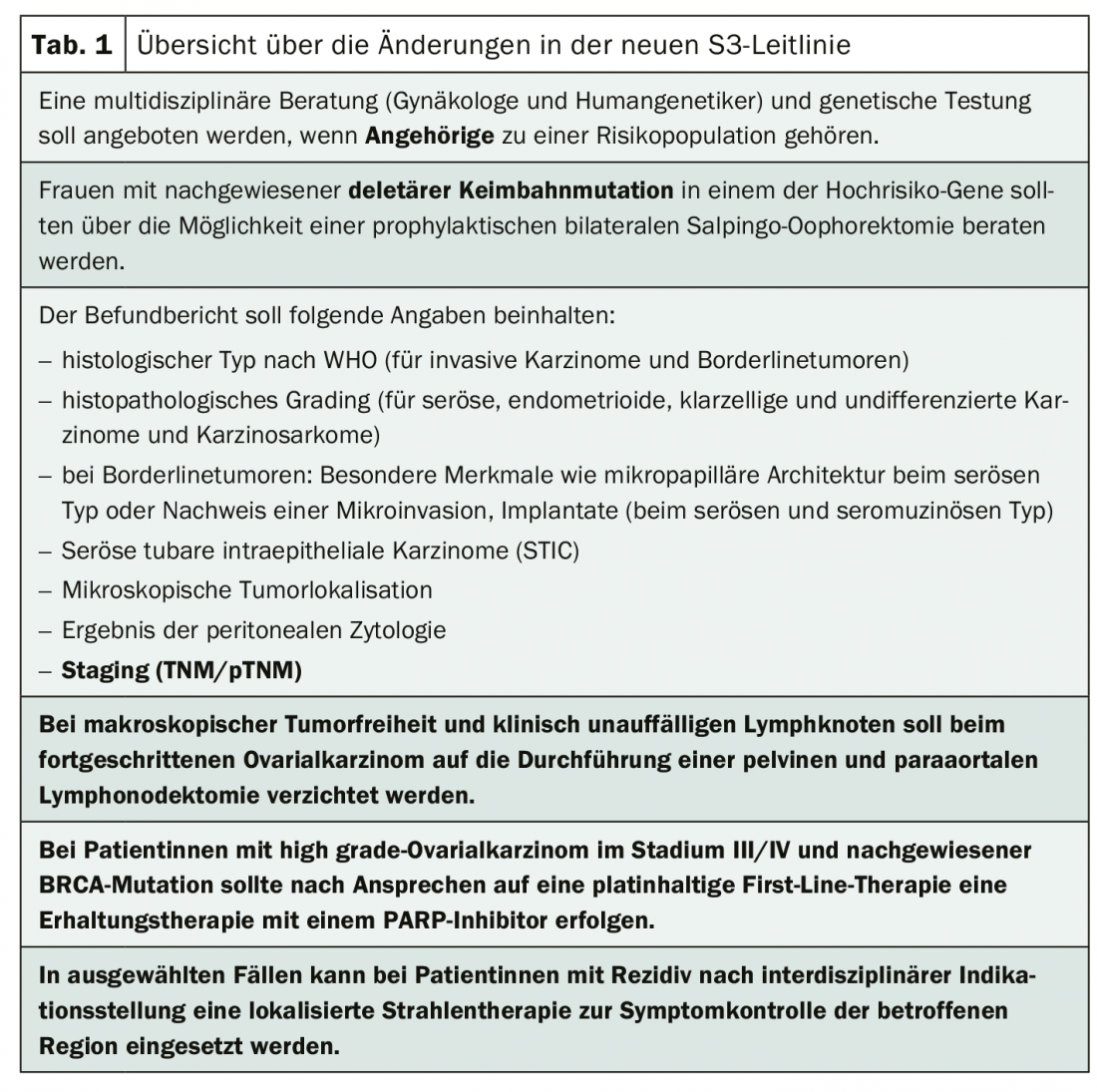
Prophylactic removal of the lymph nodes has often been considered as a medical option to generate a better prognosis for women. However, recent study results show that this intervention does not lead to an improvement in progression-free survival or overall survival. Therefore, in patients who are macroscopically tumor-free and have no clinically abnormal lymph nodes, pelvic and para-aortic lymphonodectomy should be omitted for advanced ovarian cancer.
5-10% of all patients suffering from ovarian cancer have a hereditary predisposition. The majority of genetic alterations in familial ovarian cancer syndrome are found in the BRCA1 and BRCA2 genes. In addition, there are other risk genes such as RAD51C, BRIP1, etc. The risk of disease can often be reduced by precautionary removal of the ovaries. Until now, the recommendation referred exclusively to patients with a BRCA1 or BRCA2 mutation. Now, counseling for prophylactic bilateral oophorectomy is also recommended for women who have a deletive germline mutation in one of the other known high-risk genes.
Focus on therapy optimization
Updated recommendations are also available for the use of PARP inhibitors. A randomized trial of maintenance therapy with the PARP inhibitor olaparib in BRCA1/2 mutation patients after response to carboplatin/paclitaxel in first-line therapy showed that the risk of progression or death was 70% lower than in the placebo group. Therefore, patients with aggressive stage III/IV high-grade ovarian cancer and proven BRCA mutation should receive maintenance therapy with a PARP inhibitor after platinum-containing treatment.
Since most patients with epithelial ovarian cancer have reached an advanced stage at the time of initial diagnosis, radiotherapy has not played a wesemtic role in treatment. Now there is evidence that localized irradiation of recurrences can sometimes achieve symptom and local tumor control. However, the potential benefits must be carefully weighed against the risks, and a treatment decision must be made in the context of an interdisciplinary tumor conference.
Literature:
- Burges A, Schmalfeldt B: Ovarian carcinoma. Diagnostics and therapy. Dtsch Arztebl Int 2011; 108(38): 635-641.
- Sartorius CM, Heilzelmann-Schwarz V: Epithelial ovarian carcinoma. Early detection and surgical prophylaxis. info @ gynecology 2017.
- www.leitlinienprogramm-onkologie.de/leitlinien/ovarialkarzinom
InFo ONCOLOGY & HEMATOLOGY 2020; 8(3): 29.