Restless legs syndrome is a disorder of the nervous system that causes restlessness of movement and discomfort in the legs, which mainly occurs in the evening and at night and improves with movement. Reduced sleep efficiency and interruptions to sleep can result in a relevant reduction in quality of life. Effective therapy is therefore crucial.
Restless legs syndrome (RLS) is a chronic neurological disorder that is accompanied by an intense, unpleasant urge to move the legs (rarely also in other parts of the body) and is usually accompanied by unpleasant sensations that are difficult to describe. The symptoms are particularly noticeable at night or during moments of rest. The symptoms were first described in the middle of the 17th century and then referred to as RLS, the “restless legs syndrome”, in 1945. Lying comfortably on the couch or sleeping is difficult or even impossible for those affected as the severity increases. Many patients walk around the house several times at night to relieve the symptoms. This has an enormous physical and psychological impact on those affected. It is estimated that 5-10% of the population is affected – women more often than men. The symptoms usually appear for the first time around the age of 30. Only occasionally at first, then at increasingly shorter intervals as they get older.
The underlying causes of RLS are not yet known in detail. Theories focus on an altered iron metabolism in the brain or the endogenous opioid system. There are also indications that a disorder of the dopamine metabolism in the brain could be linked to the disease. This is supported by the fact that the symptoms can often be alleviated by L-dopa or dopamine agonists. In addition to the idiopathic form, secondary or symptomatic restless legs syndrome can also occur. It then occurs in connection with other illnesses or certain circumstances, such as pregnancy. However, it is now becoming increasingly clear that this distinction is not appropriate. Because the transitions are often fluid. RLS patients often also suffer from polyneuropathy, for example. Diseases originally classified as causative, such as iron deficiency or renal insufficiency, should therefore be regarded as comorbid. It is possible that there is a genetic predisposition to RLS, but that this only comes into play because another trigger factor – such as a comorbid illness – comes into play.
Minimum criteria for RLS
The minimum criteria for suspected RLS are as follows:
- Sensory disturbances and a pronounced urge to move the limbs, especially the legs, but also the arms and other parts of the body,
- the symptoms occur when the body comes to rest,
- Exercise such as standing up, walking or stretching leads to a partial or complete improvement of the symptoms,
- the symptoms are more severe in the evening or at night than during the day or occur exclusively in the evening or at night,
- the appearance of the signs cannot be considered primarily as a symptom of another medical or behavioral cause.
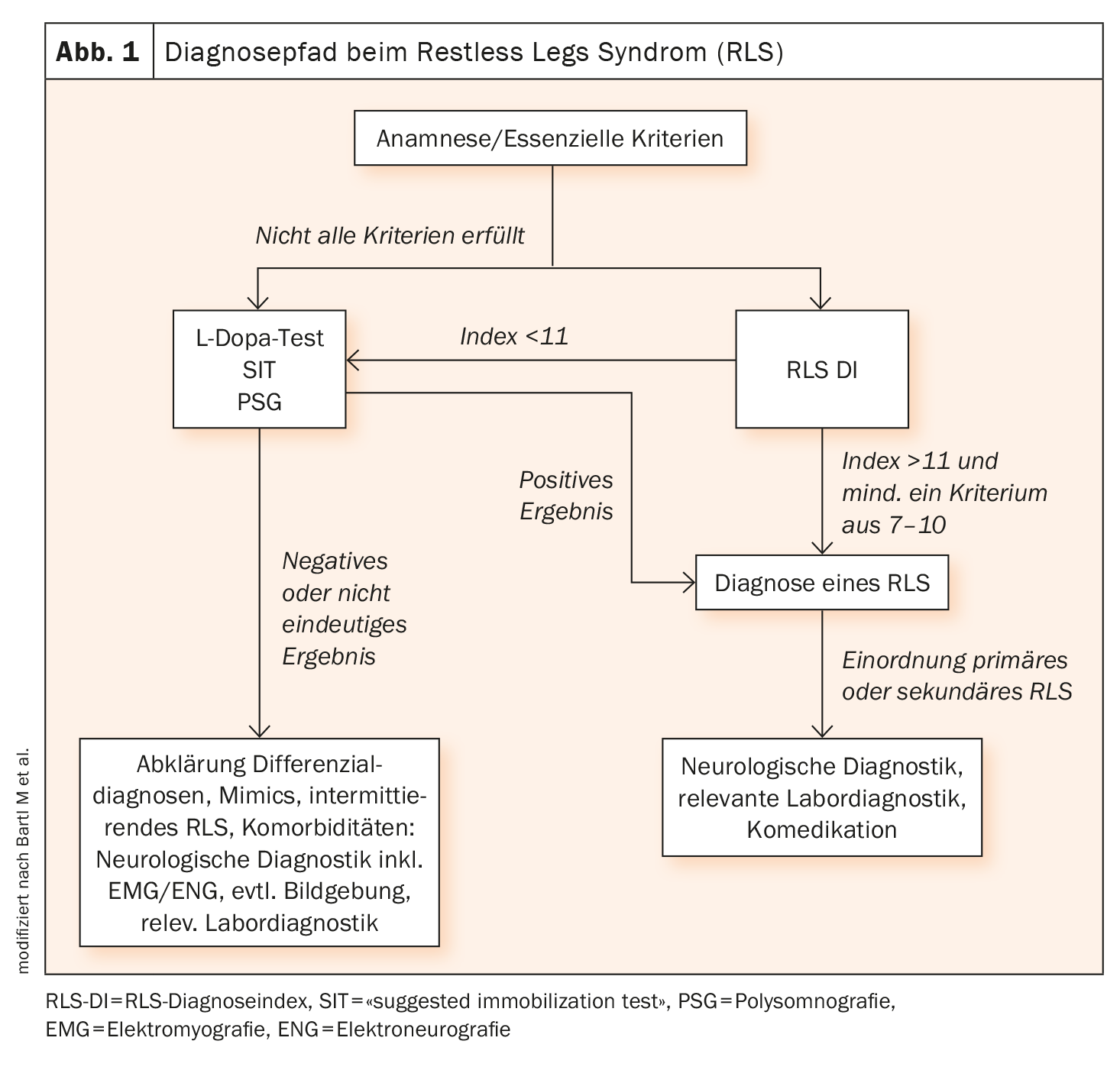
In addition, the suspicion can then be confirmed by an L-dopa test (Fig. 1). Other or comorbid diseases should be excluded. In addition to a clinical neurological examination, laboratory tests, a measurement of nerve conduction velocity, an examination in the sleep laboratory and a muscle examination can be carried out as part of further diagnostics.
Treatment management is then planned individually and adapted to the needs and symptoms of those affected. If there is a known trigger, this is addressed. Otherwise, symptomatic therapy is used. Pharmacologically, gabapentin, dopamine agonists and levodopa are the drugs of choice.
Further reading:
- www.usz.ch/krankheit/restless-legs-syndrom (last accessed on 24.01.2024)
- https://hirnstiftung.org/alle-erkrankungen/restless-legs-syndrom (last accessed on 24.01.2024)
- www.restless-legs.org/restless-legs/syndrom/allgemein (last accessed on 24.01.2024)
- Bartl M, Trenkwalder C, Muntean ML, Sixel-Döring F: (2020). Restless legs syndrome: an update. The neurologist 2020; 91(10): 955-966.
InFo NEUROLOGY & PSYCHIATRY 2024; 22(1): 38