Mechanical thrombectomy with stent retrievers for the treatment of ischemic stroke in proximal cerebral vascular occlusion is superior to intravenous thrombolysis alone. In particular, patients with proven occlusion of a proximal cerebral vessel, clinically severe neurological deficits, small infarct volume, and successful recanalization within the first six hours after symptom onset will benefit. Selected patients with proximal cerebral vessel occlusion with larger infarct volumes and in a later time window also appear to benefit from endovascular recanalization if recanalization is successful, but to a lesser extent. Currently, there are no data showing the superiority of endovascular thrombectomy without concomitant intravenous thrombolysis. Therefore, patients who qualify for intravenous thrombolysis should also receive it for proximal cerebral vascular occlusions and planned mechanical thrombectomy. The greatest treatment effect is achieved in a stroke network with an endovascular stroke center with clear referral pathways and an experienced multidisciplinary stroke team.
In the acute phase of ischemic stroke, the reopening of the occluded cerebral vessel (recanalization and reperfusion), the time from symptom onset to recanalization, and the occurrence of treatment-associated complications are among the most important factors influencing a good clinical outcome without severe disability. Successful and rapid recanalization is of greatest prognostic importance. In the course, various endovascular techniques for mechanical thrombus removal, so-called mechanical thrombectomy, have been developed. Advantages of mechanical thrombectomy include potentially faster and higher recanalization rates for proximal vessel occlusions with large thrombus burden compared with intravenous or intra-arterial thrombolysis, the possible complete elimination of thrombolytics and associated lower complication rates of symptomatic intracerebral hemorrhage, and the extension of the therapeutic time window and thus the ability to deliver treatment to more patients.
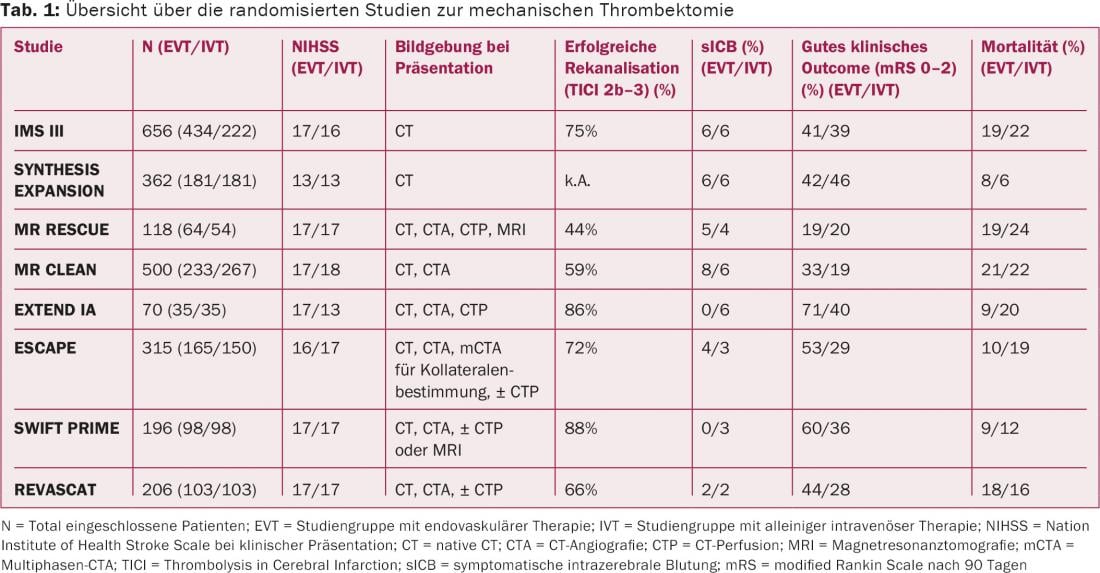
Initial mechanical recanalization techniques included endovascular advancement of an aspiration catheter anterior to the occlusion and subsequent aspiration of the thrombus (proximal thrombectomy), passing the site of occlusion and depositing corkscrew- or brush-like instruments posterior to the thrombus, thereby extracting the thrombus with withdrawal of the instrument (distal thrombectomy), and implantation of intracranial stents. These first-generation mechanical recanalization techniques were compared with the standard therapy of intravenous thrombolysis in three randomized trials (published in 2013 in the New England Journal of Medicine: IMS III, SYNTHESIS EXPANSION, MR RESCUE). However, in none of the studies was endovascular therapy superior to standard therapy in terms of clinical outcome (Table 1) [1–3].
These studies have been heavily criticized due to methodological shortcomings and their results have been doubted. In particular, the lack of sufficient cerebral imaging with dedicated vascular imaging to reliably detect proximal cerebral vessel occlusion in a large proportion of the included patients, the low patient inclusion rate of different centers over a study period of several years, and the relatively large time loss between symptom onset and endovascular intervention are criticized in these studies. However, the main criticism is directed at the almost exclusive use of first-generation mechanical thrombectomy techniques.
Stent retriever thrombectomy
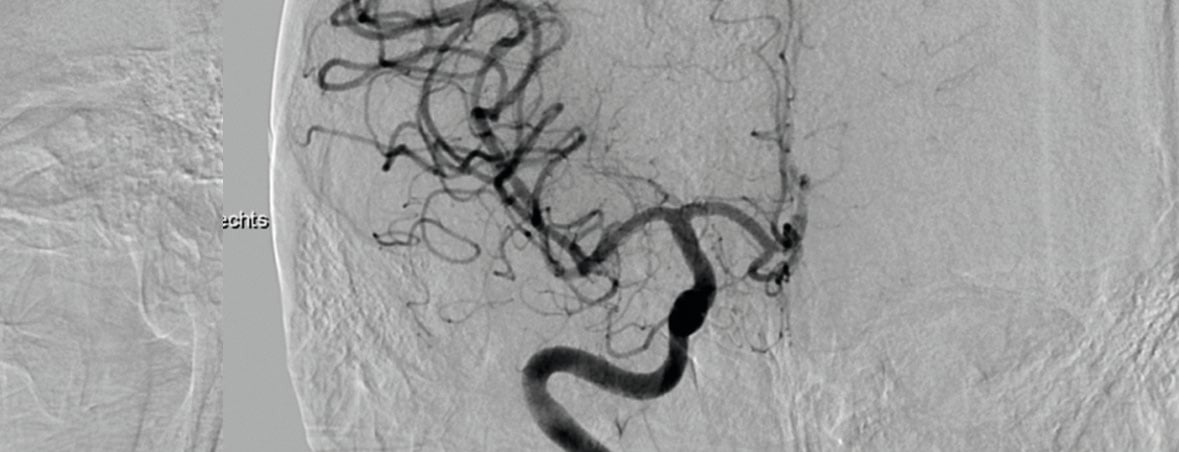
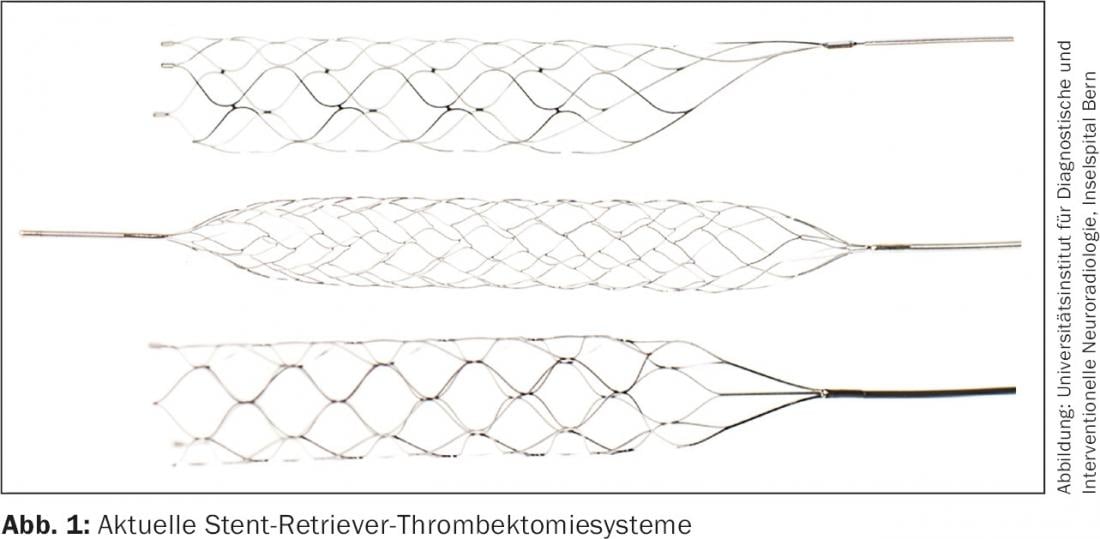
Since 2009, new thrombectomy systems, so-called stent retrievers, have been developed and introduced into clinical use. These systems are self-expandable, removable, stent-like instruments that are placed over the cerebrovascular occlusion. In the process, the thrombus becomes entangled in the stent meshes so that when the retrievable stent system is withdrawn, the thrombus can be extracted (Fig.1). Stent retriever technology combines the advantages of a classic stent with immediate restoration of flow through thrombus compression thanks to the radial force of the stent (temporary bypass effect) with the advantages of a thrombectomy system with definitive thrombus extraction even of large amounts of thrombus and with recanalization without the need to leave the system implanted on site (Fig. 2).
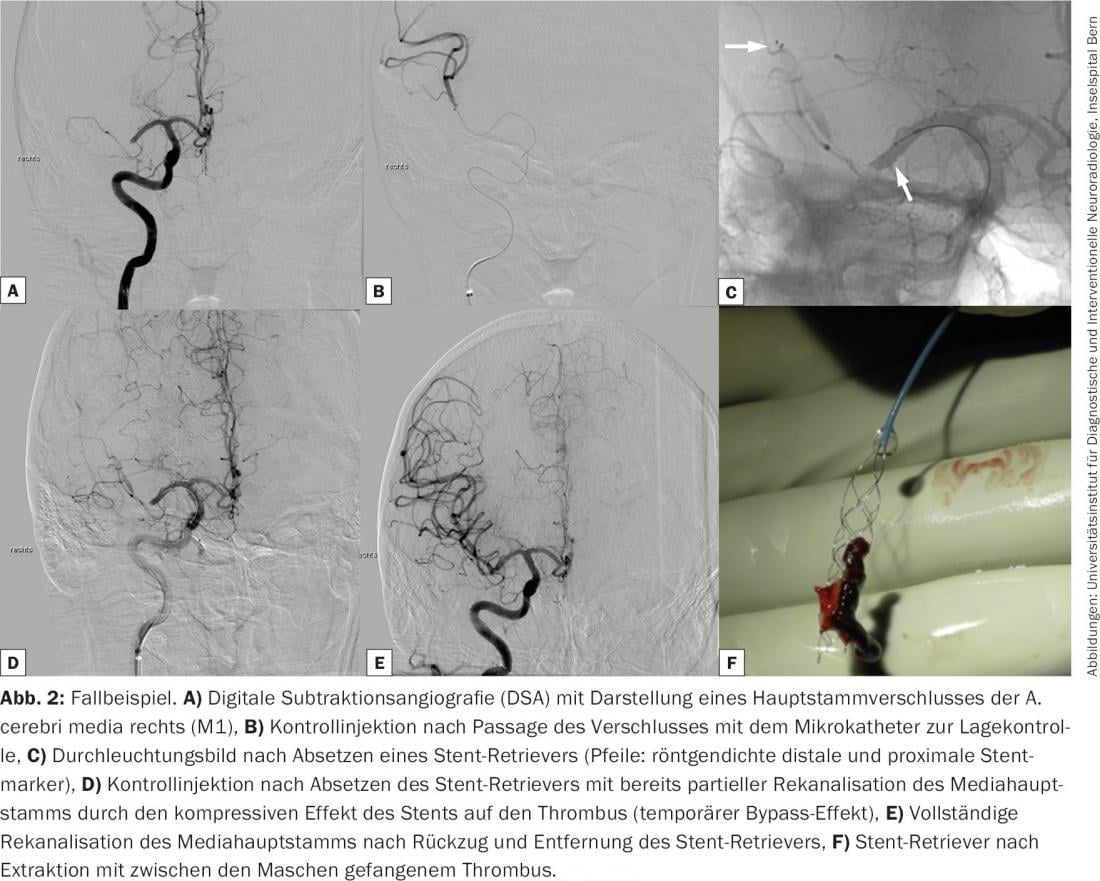
Initial clinical nonrandomized multicenter studies showed promising high rates of proximal cerebral vessel occlusion recanalization of up to 90%, short intervention times, and low complication rates, resulting in a good outcome (mRS ≤2) in up to 58% of patients [4]. In addition, prospective randomized trials demonstrated the superiority of stent-retriever thrombectomy over first-generation mechanical thrombectomy in direct comparison [5]. The unclear study situation led to several prospective randomized trials comparing intravenous thrombolysis as standard therapy and intravenous thrombolysis with additional mechanical thrombectomy with majority use of stent retrievers in acute cerebral stroke with imaging-proven proximal cerebral vessel occlusion. Five studies have now been published and provide level 1 evidence on the superiority of endovascular therapy over intravenous thrombolysis alone for proximal cerebral vessel occlusion (MR CLEAN, ESCAPE, EXTEND-IA, SWIFT PRIME, REVASCAT) [6–10].
In contrast to the previous publications, all five studies required imaging evidence of proximal cerebral vessel occlusion of the distal internal carotid artery or medial trunk by CT or MR angiography. In some studies, patients with already advanced major cerebral infarcts or poor leptomeningeal collaterals were also excluded on the basis of extended imaging criteria. In three studies, the use of a stent retriever was mandatory; in the remainder, the decision of which thrombectomy system to use was left to the interventionalist, although again, a stent retriever was used in 80% of cases. The onset of endovascular intervention had to occur within six hours of symptom onset in three studies, within eight hours in the fourth study, and within 12 hours in the fifth study; in these studies, the onset of intervention also occurred within six hours of symptom onset in more than 80% of patients.
All studies consistently demonstrated clear superiority of mechanical thrombectomy over intravenous thrombolysis alone, with high recanalization rates (TICI 2b/3 59-88%), significantly higher rates of neurologically good outcome without severe neurological disability (mRS ≤2 33-71% vs. 19-40%), and in individual studies also significantly lower mortality rates (9-21% vs. 12-22%). The number of patients who need to be treated to avoid significant neurological disability or death (Number Needed to Treat, NNT) is 3-7 in the endovascular arm. In addition, there were no increased technical complication rates and no difference in the incidence of symptomatic intracerebral hemorrhage (0-7%) (Table 1).
What conclusions can be drawn from the results?
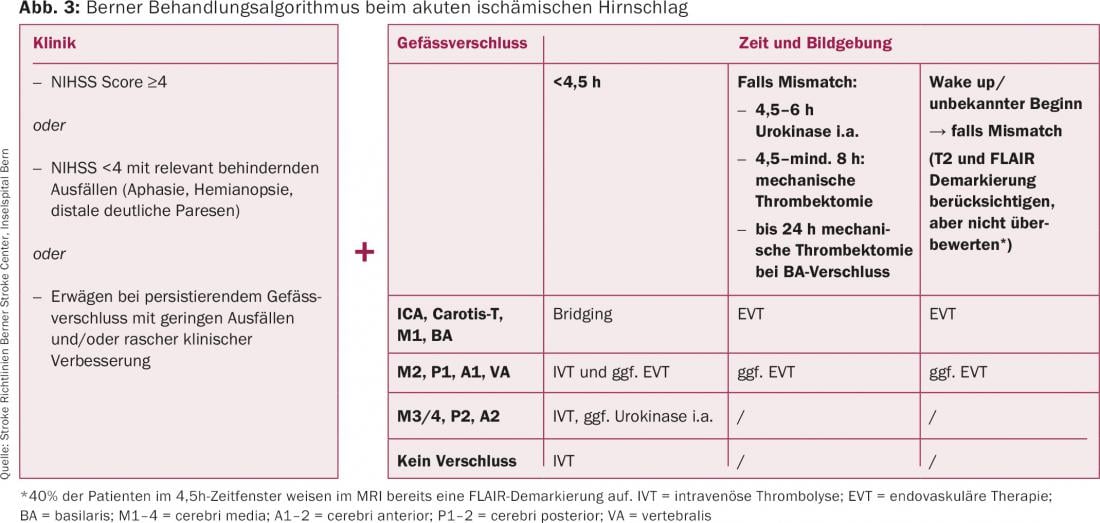
Based on these data, cerebrovascular patients with proven proximal cerebral vessel occlusions should be treated endovascularly by mechanical thrombectomy within six hours of symptom onset, if possible. Following current guidelines for ischemic stroke treatment [11,12], the Bern Stroke Center has further developed and clinically successfully implemented the decision algorithm for indication and therapy selection in acute ischemic stroke [13]. In addition to the neurological clinic and the duration since symptom onset, multimodal cerebral imaging incl. imaging of the intra- and extracranial brain-supplying vessels and perfusion imaging by CT or MRI play a decisive role in the choice of therapy. Imaging information on vessel anatomy, site of occlusion (proximal vs. peripheral), infarct size, penumbra/mismatch, and eloquence of the affected or potentially at-risk brain areas are used to make decisions (Fig. 3).
Summary
Several recently published prospective randomized trials have demonstrated the superiority of mechanical thrombectomy with second-generation thrombectomy systems (stent retrievers) in combination with intravenous thrombolysis over intravenous thrombolysis alone in acute ischemic stroke. Mechanical thrombectomy with stent retrievers resulted in very high recanalization rates, a significantly better clinical outcome, and in some cases significantly lower mortality without an increase in complication rates. In particular, patients with proven occlusion of a proximal cerebral vessel (distal internal carotid artery, main stem of the middle cerebral artery), clinically severe neurological symptoms, low infarct volume, and successful recanalization within the first six hours after symptom onset will benefit. This group of patients should be offered mechanical thrombectomy with stent retrievers as standard therapy.
Literature:
- Broderick JP, et al: N Engl J Med 2013; 368(10): 893-903.
- Ciccone A, et al: N Engl J Med 2013; 368(10): 904-913.
- Kidwell CS, et al: N Engl J Med 2013; 368(10): 914-923.
- Pereira VM, et al: Stroke 2013; 44: 2802-2807.
- Saver JL, et al: Lancet 2012; 380(9849): 1241-1249.
- Berkhemer OA, et al: N Engl J Med 2015; 372: 11-20.
- Campbell BC, et al: N Engl J Med 2015; 372: 1009-1018.
- Goyal M, et al: N Engl J Med 2015; 372: 1019-1030.
- Saver JL, et al: N Engl J Med 2015; 372: 2285-2295.
- Jovin TG, et al: N Engl J Med 2015; 372: 2296-2306.
- ESO-Karolinksa Stroke Update 2014: Consensus statement on mechanical thrombectomy in acute ischemic stroke. A collaboration of the ESO-Karolinska Stroke Update, ESMINT and ESNR. www.eso-stroke.org/eso-stroke/strokeinformation/thrombectomy-consensus-eso-karolinska-esmint-esnr.html
- Powers WJ, et al: Stroke 2015 [Epub ahead of print].
- Stroke Guidelines Bern Stroke Center. www.neurologie.insel.ch/de/unser-angebot/stroke-center/strokerichtlinien/
CARDIOVASC 2015; 14(5): 18-21