Obstructive sleep apnea affects the quality of life of those affected and is also associated with an increased cardiovascular risk. The indication for treatment results from the symptoms that occur. Diagnostic tools and therapeutic options were discussed at the SGAIM Fall Congress.
Obstructive sleep apnea (OSA) can manifest in many ways. Characteristic daytime symptoms include excessive daytime sleepiness (television sleep, car sleep), difficulty concentrating, and headaches. Nighttime symptoms include loud, irregular snoring and pauses in breathing, associated with the feeling of not having had a restful night’s sleep. Resulting complications and long-term consequences include arterial hypertension and other cardiovascular diseases, as well as an increased risk of accidents, e.g., due to falling asleep at the wheel of a car.
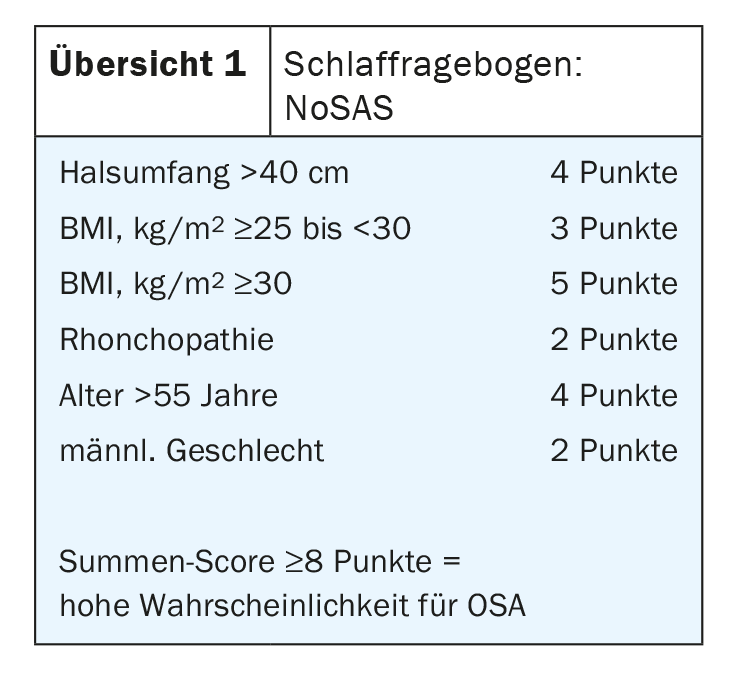
When OSA is suspected, it is advisable to distinguish between male and female patients, as the specific symptoms can be very different, explained PD Dr. Tsogyal Daniela Latshangh, Chief of Pneumology/Sleep Medicine at the Graubünden Cantonal Hospital in Chur: “Women, for example, suffer more frequently from morning headaches and fatigue, and insomnia, restless legs, depression, nightmares and palpitations also occur more frequently in them. Men, on the other hand, suffer more from snoring and observed apneas. In them, the influence of alcohol on OSA is noticeable and the discomfort increases in the supine position. To arrive at the diagnosis of OSA, the expert recommended the use of sleep questionnaires such as NoSAS or STOP Bang (Overviews 1 and 2), which usually reliably point the way.
Diagnostics
In order to diagnostically confirm the suspicion of obstructive sleep apnea, the physician has various measurement techniques at his disposal. Advanced pulse oximetry is a screening device that should be worn for at least 6 hours, and the device cannot distinguish whether the patient is asleep or awake during the wearing period. Pulse rate, oxygen saturation and respiratory rate are measured, it should only be used in cases of low pretest probability for reassurance or exclusion. If the findings are unclear, further clarification is indicated. Respiratory polygraphy is somewhat more complex, but also relatively easy and straightforward to perform on an outpatient basis.
Polysomnography is the most accurate examination represents the diagnostic gold standard, Dr. Latshangh elaborated. Again, heart rate, percutaneous O2 saturation, flow (nasal and/or oral), chest and abdominal excursion, body position, and snoring are measured. In addition, however, the EEG, ECG, EMG (M. tibialis ant, submental) and EOG å(eye movements) are measured and the whole thing is recorded on video. This can no longer be done at home, but is done in a sleep lab.

Therapeutic options
Several non-surgical and surgical methods are available to treat obstructive sleep apnea, although surgery is rarely the first option and should only be used when conservative options have been exhausted.
CPAP is still considered the gold standard, but there is a failure rate of over 35%. To achieve an effect, the mask must be worn for at least 4 hours per night on more than 80% of all nights.
Mandibular advancement splint: In the case of normal snoring, those affected must pay for the mandibular advancement splint themselves; in the case of obstructive sleep apnea, at least a portion is covered by the health insurance. The brace prevents the base of the tongue from falling back and also addresses the soft palate if necessary. The acceptance depends on the construction height and design of the rail.
Sleep position therapy: POSA (positional OSA) occurs only in mild and moderate OSAS. For treatment, for example, there are backpacks that you put on and force to the optimal position during sleep.
Behavioral measures: Weight reduction can have a positive impact on OSA: 10-15% of baseline weight less on the scale can result in a 50% reduction in AHI. Quitting smoking can also lead to improvements.
Operational options
Several options are also available for surgical therapy, including tonsillectomy, hypoglossal stimulator, tongue base reduction, epiglottopexy, or bimax. If BMI >35 kg/m2 it is advisable to consult a bariatric team.
Source: “Obstructive sleep apnea: when to diagnose, when to treat?”, PD Dr. Tsogyal Daniela Latshangh, SGAIM Fall Congress, Sept. 23, 2022.
HAUSARZT PRAXIS 2022; 17(10): 56