Patients with cardiac and/or renal insufficiency often experience electrolyte imbalance, which in many cases is life-threatening. Hyperkalemia can be caused by the underlying disease itself, but also by its treatment management. Therefore, in order not to cast out the devil with the Beelzebub, an effective approach specifically tailored to hyperkalemia is needed.
Potassium levels are determined by absorption, distribution, and (predominantly renal) elimination. On average, 1 mmol/kg is absorbed daily through food. The total concentration is then distributed with a ratio of 2% to 98% in the extracellular and intracellular space. The potassium-sodium ATPase is responsible for this. This activity can be modified via different pathways, such as insulin action or β adrenergic receptors, explained Prof. Ralph Kettritz, MD, Berlin (D). These support potassium influx into the intracellular space. Hyperglycemia, α agonists, and inorganic acidosis, on the other hand, cause potassium efflux. Potassium secretion is controlled by the mechanisms of sodium delivery, urine flow, aldosterone, and serum potassium, among others. By shifting potassium into cells and aldosterone-driven renal potassium secretion, the body can basically process high dietary potassium levels. High potassium intake also has beneficial effects on blood pressure and CV events, but also on CKD progression. According to association studies, the optimal potassium level is 4.0-4.6 mmol/l. In addition to CKD, age, diabetes mellitus, and RAAS blockade must also be considered risk factors for hyperkalemia.
The kidney in focus
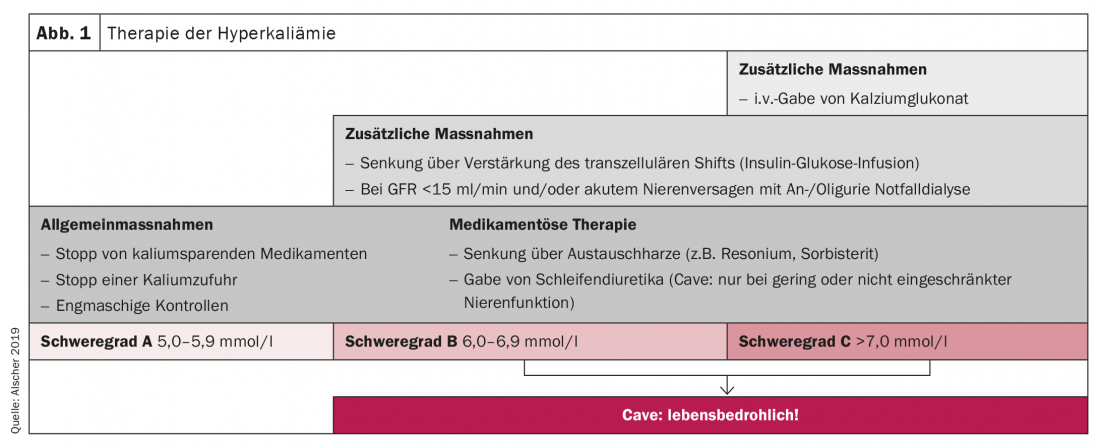
If too much potassium is supplied to the body, the appropriate countermeasures are already initiated during intestinal absorption. Prof. Dr. med. Mark Dominik Alscher, Stuttgart (D), pointed out that these mechanisms cannot fully take place in the case of impaired kidney function. In this case, acute hyperkalemia can occur very quickly. This is divided into three degrees of severity:
- Severity A: 5.0-5.9 mmol/l
- Severity B: 6.0-6.9 mmol/l
- Severity C: >7.0 mmol/l
Already from severity B the situation can be life-threatening. Accordingly, measures to lower the potassium level should be taken as soon as possible (Fig. 1).
Effects on the heart
The cardio-renal interaction in systolic heart failure resembles a vicious circle, as Prof. Christiane Angermann, MD, Würzburg (D), explained. If cardiac pump function is reduced, lower renal perfusion and diuresis are the result. This results in congestion, which in turn has an unfavorable effect on the heart. Correspondingly, the rate of hyperkalemia in heart failure increases with decreasing renal function. This leads to a core problem in practice, as this consequence is also evident depending on the therapy and therefore, for example, RAAS inhibitors are discontinued or reduced and potentially life-saving therapies are withheld, the expert said.
In this case, specific therapy of hyperkalemia should rather be considered. Sodium polystyrene sulfonate is available for this purpose, but it is subject to significant limitations, is poorly tolerated and can result in severe gastrointestinal complications. Patiromer offers significantly better tolerability with only mild gastrointestinal side effects such as constipation, as well as good study evidence, Angermann reported. Studies have shown that the potassium blocker allows initiation and up-dosing of treatment with RAAS inhibitors and thus optimized heart failure therapy.
Congress: DGIM
CARDIOVASC 2021; 20(2): 31 (published 6/27-21, ahead of print).